Abstract
The acquisition of pathogen-derived antigen by dendritic cells (DCs) is a key event in the generation of cytotoxic CD8+ T cell responses. In mice, the intracellular bacterium Listeria monocytogenes is directed from the blood to splenic CD8α+ DCs. We report that L. monocytogenes rapidly associated with platelets in the bloodstream in a manner dependent on GPIb and complement C3. Platelet association targeted a small but immunologically important portion of L. monocytogenes to splenic CD8α+ DCs, diverting bacteria from swift clearance by other, less immunogenic phagocytes. Thus, an effective balance is established between maintaining sterility of the circulation and induction of antibacterial immunity by DCs. Other Gram-positive bacteria also were rapidly tagged by platelets, revealing a broadly active shuttling mechanism for systemic bacteria.
Similar content being viewed by others
Main
Dendritic cells (DCs) are strategically positioned within organs and tissues to optimize the chances of antigen encounter. In the spleen, DCs survey the bloodstream and form an integral part of the reticuloendothelial system, a network of phagocytic cells from the spleen and liver that capture antigens, including viruses and bacteria. Macrophages constitute the majority of phagocytic cells in the reticuloendothelial system, and their chief role is to clear and destroy captured particles. DCs, in contrast, 'preserve' antigenic information to initiate immune responses1. Consequently, the spleen actively contributes to maintaining sterility of the bloodstream, and the captured material simultaneously serves as an immediate source of antigen for the developing immune response. Opsonization with complement and antibody facilitates the localization of circulating antigen to the spleen2,3, and aids its deposition in the dense network of specialized macrophages, B cells and DCs known as the marginal zone4. Among the DCs in the marginal zone are CD8α+ DCs5, a subset that has important roles in cross-presentation, homeostasis and tolerance. In addition, CD8α+ DCs collaborate with marginal zone macrophages in the generation of cytotoxic CD8+ T cell responses6.
Effective CD8+ T cell responses are vital for controlling intracellular pathogens such as Listeria monocytogenes. Infection of mice with this well-characterized, Gram-positive, facultative intracellular bacterium (which can cause severe septic infections in neonates, pregnant women or immunocompromised people) has contributed to the understanding of T cell–mediated immunity7. DCs are indispensable for the induction of anti-listerial CD8+ T cell immunity8,9 and recall responses10, enabling individual naive L. monocytogenes–specific CD8+ precursor T cells to proliferate and differentiate into a full range of effector and memory T cell populations11. Furthermore, CD8α+ DCs are the principal DC subset that initiates L. monocytogenes–directed CD8+ T cell immunity12. Notably, the splenic CD8α+ DC population also provides systemic L. monocytogenes with an early survival niche and forms the origin of further bacterial spread13,14. Systemic L. monocytogenes are rapidly transported to the marginal zone of the mouse spleen13,15 and are taken up by CD8α+ DCs. Subsequently, L. monocytogenes escape the phagolysosome and spread to adjacent cells and the rest of the organ, propelled by a mechanism of actin polymerization. Thus, DCs have a dual role during L. monocytogenes infection: they are vital for the induction of effective T cell immunity, but they also allow colonization by L. monocytogenes. Splenectomized mice show greater resistance to infection with L. monocytogenes16, which illustrates this dual role of the spleen and its DCs.
Because CD8α+ DCs have a crucial role in infection and immunity, we set out to determine the factors that guide systemic bacteria to this spleen-resident cell type. We used the ability of L. monocytogenes to survive within CD8α+ DCs, which, in combination with sorting of splenocytes from infected mice by flow cytometry, allowed us to detect rare and viable intracellular bacteria within defined splenocyte subsets under different experimental conditions17. We found that L. monocytogenes associated with platelets in the circulation, and that this association was required for efficient shuttling of bacteria to CD8α+ DCs in the spleen. Moreover, association between platelets and L. monocytogenes was mediated by the covalent opsonizing complement factor C3, and platelet receptor GPIb was critically involved in this interaction. C3-mediated platelet association was common among diverse Gram-positive bacteria, including species of clinical relevance. Absence of complement-mediated platelet association led to accelerated clearance of L. monocytogenes from the bloodstream. Thus, platelet adherence balances rapid destruction of systemic bacteria by phagocytes of the reticuloendothelial system, while diverting a small but important portion of viable bacteria to the immunity-inducing CD8α+ DC compartment. Indeed, we observed significantly lower antibacterial cytotoxic CD8+ T cell responses in experimental settings in which L. monocytogenes could not adhere to platelets and effectively reach CD8α+ DCs. Moreover, our data clarify bacterial adherence in the circulation during Gram-positive bacteremia.
Results
Complement allows spleen colonization by L. monocytogenes
Systemic L. monocytogenes rapidly localize to the splenic marginal zone and infect CD8α+ DCs, which are then used as a starting point for the spread of bacteria to other splenocytes and consequently the entire organ13,14,15. Because the complement system influences the clearance of bacteria from the bloodstream and their localization to the spleen2, we determined whether complement was involved in targeting L. monocytogenes to splenic CD8α+ DCs. Thus, we screened the degree of splenic L. monocytogenes colonization in mice specifically lacking the covalent opsonizing factor C3, the most abundant and central factor of the complement system.
We found that during the course of infection, bacterial burdens in the spleen were much lower in C3−/− mice than in C3+/+ wild-type control mice. After 1 d of infection, bacterial burdens in the spleens of C3−/− mice were significantly lower than those in wild-type mice (Fig. 1a). Ineffective colonization of the spleen without a functioning complement system was most evident at 3 d after inoculation, when bacterial concentrations peaked in wild-type mice but in C3−/− mice remained in a range similar to that observed on day 1 (Fig. 1b). We administered an infectious dose that C57BL/6 wild-type mice overcome within 7 d (0.1 of the median lethal dose), and accordingly both mouse strains had no detectable bacterial infection at that time point (Fig. 1c). Although the lower bacterial burden in C3−/− mice might seem counterintuitive given the well-established role of the complement system in thwarting microbial infection via opsonization and lysis, these findings led us to hypothesize a complement-dependent shuttling pathway for L. monocytogenes to its early survival niche.
(a–c) Splenic L. monocytogenes burden in C3−/− or C3+/+ wild-type (WT) mice at 1 d (a), 3 d (b) or 7 d (c) after intravenous infection. (d) Enzyme-linked immunosorbent assay (ELISA) of the systemic depletion of C3 from serum by CVF at t = 0. (e) Splenic L. monocytogenes burdens at 3 d after infection in mice depleted of C3 by CVF injection starting before (t = −20 h, −1 h and +20 h; middle) or shortly after (t = +30 min and +20 h; right) L. monocytogenes infection (t = 0), compared with control wild-type mice (left). (f) Splenic L. monocytogenes burdens in C3ar1−/− or wild-type mice 3 d after intravenous infection. Dashed lines indicate detection limit (a–c,e,f) or 50% of maximum absorbance (d). NS, not significant. P values, unpaired, two-tailed Student's t-test. Data represent two or more independent experiments (mean ± s.d. of three or more mice).
To verify the role of complement during early L. monocytogenes infection, we depleted wild-type mice of C3 by systemic administration of cobra venom factor (CVF), which diminished circulating C3 to ∼10% of the normal wild-type concentration (Fig. 1d). In addition to serving as a transient depletion model, independent of genetic C3 deficiency, CVF treatment allows control over the time frame of C3 deficiency. In this manner, we found that C3 depletion starting before infection (a situation simulating genetic C3 deficiency) resulted in greater resistance to L. monocytogenes infection, as shown by significantly lower spleen burdens 3 d after infection (Fig. 1e). In contrast, C3 depletion starting shortly after inoculation did not enhance resistance to L. monocytogenes (Fig. 1e). Thus, transient C3 depletion with CVF before infection confirmed our finding of enhanced resistance of genetically C3-deficient mice to L. monocytogenes (Fig. 1b), whereas depletion immediately after infection indicated a role for C3 during the earliest phases of infection.
In addition to covalent opsonization with C3b, activated C3 also gives rise to anaphylatoxin C3a, which promotes inflammation and chemotaxis. To exclude the possibility that greater resistance of C3−/− and CVF-depleted mice to L. monocytogenes infection was due to the action of C3a, rather than opsonizing C3b, we subjected mice deficient in the receptor for C3a (C3ar1−/−) to the same infection protocol. We assessed splenic L. monocytogenes burdens at day 3 after infection and found no difference between C3ar1−/− mice and wild-type control mice (Fig. 1f), which excluded the possibility that C3a was the complement activation product relevant to the observed phenotype. Instead, these results indicated that during the earliest moments of systemic infection, opsonic C3 promotes splenic colonization with L. monocytogenes.
CD8α+ DCs gain access to systemic bacteria via complement
Given the crucial role of CD8α+ DCs in colonization of the spleen14, the results reported above (Fig. 1) were consistent with a role for complement in directing blood-borne L. monocytogenes to splenic CD8α+ DCs. To assess the influence of C3 on early splenic infection and cellular tropism, we generated wild-type or C3−/− serum-opsonized L. monocytogenes inoculums for administration into C3−/− mice. In vitro incubation of L. monocytogenes with serum from wild-type mice led to deposition of C3 onto the bacterial surface, but incubation with serum from C3−/− mice did not (Fig. 2a), as has been reported18. Moreover, opsonization did not affect bacterial viability, and we retrieved equal numbers of viable L. monocytogenes from each respective inoculum (Fig. 2b). As early as 1 h after infection, thus well before we expected substantial bacterial replication, we detected lower bacterial burdens in spleens of C3−/− mice when the L. monocytogenes inoculum had been incubated in C3−/− serum than when the inoculum was incubated with wild-type serum (Fig. 2c).
(a) ELISA of C3 concentrations in wild-type and C3−/− sera (left) used to preincubate L. monocytogenes in vitro; inoculums were washed by repeated centrifugation and resuspension until the ELISA signal from the final wash approached background (middle), which ensured that the C3 signal from the inoculum represented deposited, not soluble, C3 (right). (b) Viability of L. monocytogenes inoculum after preincubation in wild-type or C3−/− serum, assessed by plating on brain-heart infusion (BHI) agar and overnight incubation at 37 °C. (c) Early splenic L. monocytogenes burdens of C3−/− mice 1 h after infection with L. monocytogenes incubated with C3−/− or wild-type serum. (d) Spleens of C3−/− mice obtained 1 h after infection with C3−/− or wild-type serum-incubated L. monocytogenes. Splenic CD11cloCD8αloCD11b+ granulocyte (PMN) and macrophage (Mφ, including monocytes) populations were segregated from CD8α+ and CD8α− CD11c+ DC populations by flow sorting, and sorted populations were lysed and plated onto BHI agar to determine degree of infection. Total spl, total splenocytes. Dashed line in b,c, detection limit. P values, unpaired, two-tailed Student's t-test. Data represent three independent experiments (mean ± s.d. of three or more mice).
Next we used the ability of L. monocytogenes to survive within CD8α+ DCs and flow cytometry–sorted various phagocytic cell populations from spleens of C3−/− mice at 1 h after they had been inoculated with wild-type or C3−/− serum-opsonized L. monocytogenes, respectively. Subsequently, the sorted populations were lysed and we assessed the colony-forming units arising from them. This approach sensitively detects rare and viable intracellular bacteria in defined splenocyte subsets17. In confirmation of earlier studies14, CD8α+ DCs were an early niche of L. monocytogenes and we cultured only a few bacteria from macrophages and CD8α− DCs. However, we cultured only a few bacteria from CD8α+ DCs when we incubated the inoculum in C3−/− serum rather than wild-type serum (Fig. 2d), which indicated that C3 was a key factor promoting early establishment of L. monocytogenes in the spleen.
Complement mediates L. monocytogenes–platelet association
Our aforementioned experiments of timed C3 depletion (Fig. 1e) or sorting of infected CD8α+ DCs (Fig. 2d) suggested a role for C3 in the early stages of infection. C3 is abundant in the circulation and may thus opsonize bacteria immediately upon their entry into the bloodstream. We therefore analyzed the appearance of L. monocytogenes marked with the cytosolic dye CFSE in the peripheral blood of wild-type or C3−/− mice within 1 min of systemic infection. Notably, essentially all L. monocytogenes recovered from the circulation of wild-type mice was associated with cellular components positive for the platelet membrane glycoprotein IIb (CD41), whereas this exclusive association with platelets was lost in C3−/− mice (Fig. 3a). The limited residual L. monocytogenes–platelet coacquisition in C3−/− mice reflected the overall CD41+/CD41− ratio of the sample (Fig. 3a), consistent with the proposal that these events occurred by chance owing to acquisition of a free platelet and free bacterium within the same droplet, a technical problem in the detection of such small particles. We further investigated L. monocytogenes association with platelets using fluorescence microscopy and found small clusters of about one to five platelets per L. monocytogenes in the blood obtained from infected wild-type mice; in contrast, we observed no clustering in the blood from infected C3−/− mice (Fig. 3a). Notably, platelet association was rescued in C3−/− mice by preopsonizing the L. monocytogenes inoculum with wild-type serum, or inhibited in wild-type mice by pretreating the mice with CVF (Fig. 3b). Together, these data identify a highly specific, rapid and C3-dependent association of L. monocytogenes with platelets in the bloodstream.
(a) Flow cytometry (left and middle) and fluorescence microscopy (right) of blood samples of wild-type mice (top) or C3−/− mice (bottom) obtained within 1 min of infection with CFSE-marked L. monocytogenes (middle, right) or left uninfected (left). Platelets, red; L. monocytogenes, green. Scale bars, 5 μm. (b) Flow cytometry of L. monocytogenes–platelet interactions in wild-type mice treated with CVF before infection (top right) and untreated controls (top left) or in C3−/− mice infected with L. monocytogenes incubated with wild-type serum (bottom left) or C3−/− serum (bottom right). (c) Flow cytometry analysis of L. monocytogenes–platelet interactions with (left) or without (right) classical and MBL-pathway-enabling complement C4. (d) Flow cytometry analysis of normal L. monocytogenes–platelet interactions in mice lacking immunoglobulin (Rag1−/−) or complement components C1q or C5. (e) In vitro blocking assay of hirudinated C4b−/− whole blood and monoclonal antibodies to specified platelet surface molecules. (f) Flow cytometry analysis of blood obtained from GpIba−/− and C4b−/− mice within 1 min of intravenous infection with CFSE-marked L. monocytogenes. (g) Flow cytometry sorting of cells from spleens of Gp1ba−/− and wild-type mice collected 1 h after infection with L. monocytogenes; sorted CD11cloCD8αloCD11b+ granulocyte (PMN) and macrophage (Mφ, including monocytes) and CD8α+ and CD8α− CD11c+ DC populations were lysed and plated onto BHI agar to determine degree of infection. In a–d,f, numbers below plots at right relate to bacterial gate (right) and show percentage of total L. monocytogenes that are either associated (top) or not associated (bottom) with CD41+ platelets (together 100%). Numbers at left relate to nonbacterial gate (left) and show percent CD41+ platelet events (top) versus nonplatelet events (bottom) (together also 100%). Data represent two to three independent experiments.
Complement factor C3 is a central component of the complement system, and it can become activated via several pathways. We examined platelet-bacteria association in mice selectively lacking complement C4, a key factor of the 'classical' and 'mannose-binding lectin' pathways of complement activation. The absence of C4 (C4b−/−) did not interfere with the ability of L. monocytogenes to associate with platelets (Fig. 3c), confirming a dominant role for C3 and the 'alternative' pathway of complement activation in opsonizing the bacteria18. Complement C5 (in the presence of immunoglobulins) and the receptor for the globular domain of C1q have been implicated in in vitro models of bacteria-platelet interaction19,20,21. We excluded the possibility of a role for C1q, immunoglobulins and C5 in vivo using C1qa−/− mice, recombination-activating gene 1 (Rag1−/−) mice and naturally C5-deficient mice, respectively (Fig. 3d), which confirmed that a previously unknown type of bacteria-platelet interaction is involved in shuttling bacteria from the circulation to CD8α+ DCs.
Next, we set out to identify platelet surface molecules involved in the interaction between platelets and L. monocytogenes. In an in vitro assay using a panel of monoclonal antibodies specific for a range of abundantly expressed platelet markers in whole C4b−/− blood (to preclude the possibility of classical pathway–mediated complement activation on platelets while principally supporting the possibility of L. monocytogenes–platelet association), we identified a GPIb α-specific clone (p0p/B)22 that abrogated L. monocytogenes–platelet interaction (Fig. 3e). We confirmed involvement of GPIb in a mouse line lacking normal surface expression of this molecule (Gp1ba−/−)23 (Fig. 3f). Notably, lack of GPIb on platelets led to impaired shuttling of L. monocytogenes to CD8α+ DCs (Fig. 3g).
Platelet adhesion promotes bacteria targeting to CD8α+ DCs
The above experiments indicated that adhesion of platelets to L. monocytogenes is a crucial step in [the infection of CD8α+ DCs. We therefore expected that the absence of platelets would lead to less in vivo targeting of this cell population and lower spleen burdens than in the presence of platelets, which would mirror the results obtained with C3−/− mice (Fig. 1). To address this hypothesis, we depleted complement-sufficient wild-type mice of platelets in vivo and sorted macrophages and DCs from the spleens 1 h after infection to assess their bacterial content. Indeed, lack of platelets resulted in considerably fewer L. monocytogenes in splenic CD8α+ DCs (Fig. 4a). Consistent with that early decrease, total splenic bacterial burdens of platelet-depleted mice were also lower 3 d after infection (Fig. 4b).
(a) Spleens of platelet-depleted wild-type mice (WT – plt) and control wild-type mice obtained 1 h after L. monocytogenes infection. Splenic CD11cloCD8αloCD11b+ granulocyte (PMN) and macrophage (Mφ, including monocytes) populations were segregated from CD8α+ and CD8α− CD11c+ DCs by flow sorting, and the sorted populations, as well as unsorted splenocytes (Total spl), were lysed and plated onto BHI agar to determine degree of infection. (b) L. monocytogenes spleen burdens at 3 d after infection in platelet-depleted wild-type and control wild-type mice. Dashed line, detection limit. (c) Intracellular flow cytometry analysis for platelet marker CD41 within splenocyte populations, including CD8α+ and CD8α− CD11c+ DCs (left and right, respectively) for indicated L. monocytogenes doses. (d) Summary of intracellular and surface CD41 staining (left and right, respectively) for all sorted splenocyte populations and L. monocytogenes doses. P values, unpaired, two-tailed Student's t-test. Data represent two to three independent experiments (mean ± s.d. of three or more mice).
Not only L. monocytogenes (Fig. 2d) but also platelets were specifically taken up by CD8α+ DCs: intracellular detection of the platelet-specific marker CD41 steadily increased in the CD8α+ DC compartment with incremental intravenous doses of L. monocytogenes (Fig. 4c, left). The CD41 signal did not increase in the other phagocytic splenocyte fractions analyzed (Fig. 4d, left), including CD8α− DCs (Fig. 4c, right), nor did we detect it when we omitted cell permeabilization and considered only cell surface detection (Fig. 4d, right). Together these data indicate that complement-mediated platelet adherence facilitates the targeting of L. monocytogenes to its early splenic CD8α+ DC survival niche.
Less CD8α+ DC targeting and antibacterial immunity
Next we assessed the influence of complement-platelet-mediated CD8α+ DC targeting on the induction of L. monocytogenes–directed T cell immunity. To limit bacterial spread and thus exclude the possible involvement of successive cohorts of antigen-presenting cells in the induction of T cell responses, we infected mice with a mutant L. monocytogenes strain–deficient in spreading. Genetic deletion of the ActA protein (ΔActA), which is responsible for the actin-based motility of L. monocytogenes in mammalian cells, prevents the spreading of L. monocytogenes beyond the initially targeted CD8α+ DCs. Moreover, the mutant strain also transgenically expresses chicken ovalbumin, which allows assessment of defined infection-specific cytotoxic T cell responses to this surrogate bacterial antigen. In C3−/− mice, efficient CD8α+ DC targeting via bacterial adhesion to platelets cannot occur, and coincidentally ovalbumin-directed (H2-Kb–SIINFEKL multimer–positive) CD8+ T cell responses to L. monocytogenes–ovalbumin-ΔActA infection were significantly lower than those in wild-type mice (Fig. 5a). However, C3−/− mice were principally able to mount robust CD8+ T cell responses to infection, as we found with ovalbumin-expressing replication-deficient modified vaccinia Ankara (Supplementary Fig. 1), whereas platelet depletion in complement C3–sufficient mice led to impaired CD8+ T cell responses to L. monocytogenes–ovalbumin-ΔActA (Fig. 5b). Also, populations of adoptively transferred ovalbumin-specific T cell antigen receptor (TCR)-transgenic CD8+ T cells (OT-I cells), derived from complement-sufficient mice, expanded poorly in an environment in which bacteria-platelet association and efficient CD8α+ DC targeting cannot occur (Fig. 5c). These data are consistent with a requirement for blood-borne L. monocytogenes to associate with platelets to generate optimal antibacterial responses.
(a,b) Flow cytometry of splenic CD8+ T cells from wild-type (left) and C3−/− mice (right; a) or platelet-depleted wild-type mice (right; b) 7 d after infection with spreading deficient (ΔActA) ovalbumin-expressing L. monocytogenes. Numbers above outlined areas indicate percent H2-Kb–SIINFEKL multimer–positive (ovalbumin-specific) cells. (c) Flow cytometry analysis of the frequency of adoptively transferred (day −1) CD90.1+ ovalbumin-specific TCR-transgenic OT-I T cells into wild-type (left) versus C3−/− mice (right) subjected to same infection protocol as a,b. Middle and right (a–c), average H2-Kb–SIINFEKL multimer–positive CD8+ T cells (a,b) or OT-I T cells (c) among of all CD8+ T cells (middle) or absolute number (right) per spleen. P values, unpaired, two-tailed Student's t-test (a–c). Data are represent two to three independent experiments (mean ± s.d. of three or more mice).
Platelets balance clearance with immunity induction
The reticuloendothelial system of professional phagocytes has an important role in the filtration and clearing of the circulation. As viable L. monocytogenes accumulate in spleen-residing CD8α+ DCs (Fig. 2d), we assessed the relative contribution of DC phagocytosis in the overall clearance of systemic L. monocytogenes. Despite their central role in both the establishment14 and resolution of L. monocytogenes infection8, we found the contribution of DCs in L. monocytogenes clearance to be insubstantial, as the clearance kinetics were identical in wild-type mice and the CD11c-DTR mouse model of DC depletion (Fig. 6a and Supplementary Fig. 2a). In contrast, we found that clearance without C3 was significantly accelerated (Fig. 6b), which was unexpected given the established role of complement in early bacterial clearance2. The accelerated clearance in C3−/− mice could, however, be fully attributed to reticuloendothelial system phagocytes, as the depletion of macrophages by systemic clodronate liposome treatment abrogated clearance entirely (Fig. 6c and Supplementary Fig. 2b).
(a–d) Vascular clearance of L. monocytogenes in minutes after intravenous injection into wild-type and DC-depleted CD11c-DTR mice (a), wild-type and C3−/− mice (b), macrophage-depleted and control C3−/− mice (c) or platelet-depleted and control wild-type mice (d). (e) Vascular clearance of L. monocytogenes after intravenous injection into wild-type, C3−/− and platelet-depleted wild-type mice, presented as linear regression best-fit slope (actual values in parentheses) over the first 5 min after infection. (f) Kinetics of the clearance of L. monocytogenes after intravenous injection. *P < 0.05, **P < 0.01 and ***P < 0.001 (unpaired, two-tailed Student's t-test). Data represent two to five independent experiments (mean ± s.d. of three or more mice).
To determine whether complement-mediated platelet adhesion 'shielded' L. monocytogenes from rapid intravascular clearance, we assessed bacterial clearance in platelet-depleted wild-type mice. Compared with the clearance of wild-type controls, platelet-depleted wild-type mice showed an initial accelerated clearance similar to that in infected C3−/− mice (Fig. 6d and Supplementary Fig. 2c), at a rate double that of wild-type controls (linear regression best-fit values over the first 5 min were −0.21 ± 0.048, −0.44 ± 0.067 and −0.47 ± 0.052 for wild-type, C3−/− and platelet-depleted wild-type mice, respectively; Fig. 6e). As a result, >90% of the inoculum was cleared within the first 3 min in both C3−/− and platelet-depleted wild-type mice, whereas wild-type mice reached this degree of clearance in 5–10 min (Fig. 6f). Complement-mediated platelet binding seemed to shield L. monocytogenes from rapid destruction in the reticuloendothelial system, promoting DC targeting (Figs. 2d,3g and 4a) cell immunity (Fig. 5).
Platelet association is common among Gram-positive bacteria
To test whether C3-promoted platelet association is a unique feature of L. monocytogenes or a more general mechanism, we assessed platelet adhesion to a variety of other Gram-positive bacterial strains, including several that can cause severe infection in the absence of a functional complement system24,25. Similar to results obtained with L. monocytogenes, we observed 'preferential' platelet association for Staphylococcus aureus, Enterococcus fecalis and Bacillus subtilis in wild-type mice, whereas coacquisition in C3−/− mice was a chance event that reflected the overall CD41+/CD41− ratio (Fig. 7). We did not observe specific platelet association with Streptococcus pneumoniae, the only encapsulated strain tested within the panel, consistent with the reported ability of its capsule to effectively inhibit complement deposition onto its surface26. Indeed, nonencapsulated S. pneumoniae, derived from the same parental strain, regained exclusive platelet binding (Fig. 7). Together, these data show that bacteria-platelet association is dominated by C3 and is a common feature among Gram-positive bacteria.
Flow cytometry analysis of blood samples of wild-type (top) or C3−/− mice (bottom) obtained within 1 min of infection with CFSE-marked S. aureus, E. fecalis, B. subtilis or encapsulated or noncapsular forms of S. pneumoniae. Below plots: right (bacterial gate), frequency of total bacteria associated (top) or not associated (bottom) with CD41+ platelets (together 100%); left (nonbacterial gate), frequency of CD41+ platelet events (top) or nonplatelet events (bottom; together, 100%).
Discussion
The complement system is involved in innate and acquired immune responses to diverse infections in humans and mice24,25,27. In line with this well-established role, complement enhances L. monocytogenes phagocytosis28, aids L. monocytogenes–specific T cell responses29, and mice lacking complement receptor 3 (ref. 30) or the immunoglobulin superfamily complement receptor31 are more susceptible to L. monocytogenes infection. Even so, our findings show that L. monocytogenes also exploits the complement system and requires it to establish itself in the host spleen by initially targeting, surviving in and spreading from CD8α+ DCs. In a clinical setting, this facultative intracellular character enables L. monocytogenes to migrate across the placenta or blood-brain barrier, which makes it a serious health hazard to pregnant women or immunocompromised people7. In our experimental setting, we used the intracellular survival strategy of L. monocytogenes as a tool to sensitively detect live bacteria in flow-sorted splenocyte populations, enabling us to identify a complement- and platelet-based 'delivery mechanism' to CD8α+ DCs. Moreover, we identified a crucial role for platelet receptor GPIb in this shuttling pathway. In the case of systemic L. monocytogenes, this targeting route represents a double-edged sword to the host: whereas blood-borne bacteria are shuttled to a potent immunity-inducing DC population, that same population simultaneously provides L. monocytogenes with an early survival niche. Identification of this shuttling system for blood-borne bacteria therefore also provides mechanistic detail for reports that have identified the importance of the spleen16 and its DC populations13,14 in facilitating L. monocytogenes infection.
More generally, the findings described here outline a complement- and platelet-based mechanism that provides CD8α+ DCs with access to bacterially derived antigenic material from the circulation. Indeed, when L. monocytogenes targeting to splenic CD8α+ DCs is impaired in the absence of complement-mediated platelet adhesion, infection-directed T cell immunity becomes much lower. Our data thus provide a plausible mechanism for the diminished L. monocytogenes–specific T cell responses that have been described in C3−/− mice29. C3-dependent platelet association was not limited to L. monocytogenes but was also found in other unrelated Gram-positive bacteria, which suggests that this mechanism may be generally important, and possibly supporting key CD8α+ DC functions such as cross-presentation of exogenous antigen or capture of apoptotic cells.
We also conclude that bacterial association with platelets balances two vital processes: restoring sterility of the circulation through rapid destruction of systemic bacteria by reticuloendothelial system phagocytes, and shifting a small portion of bacteria to CD8α+ DCs to induce infection-specific immunity. How this balance is achieved on a cellular and molecular level remains unclear, but, consistent with our findings, pathogen-associated molecular patterns of C3-opsonized bacteria could become partially 'shrouded' by adhering platelets, delaying pathogen-specific recognition and clearance by reticuloendothelial system phagocytes. Simultaneously, the greater size of such clusters, relative to the size of a single bacterium, might favor capture within the cell-packed marginal sinus, where blood slowly percolates through the spleen and a substantial population of CD8α+ DCs resides4,5. As for this hypothesis, a published study has described an effective collaboration between marginal zone macrophages and CD8α+ DCs in the generation of cytotoxic CD8+ T cells6.
Bacteria-platelet interactions have attracted interest for several reasons, including the bactericidal properties of platelets, bacterial contamination of transfusion platelets, infective endocarditis and thrombocytopenia32. For many strains, host or bacterial factors mediating platelet interaction remain unidentified, but for some, involvement of the complement system has been suggested32. One study has described the binding affinity of S. aureus protein A to gC1qR-p33, the predominantly intracellular C1q receptor21. Affinity of gC1qR-p33 has also been described for InternalinB33, an L. monocytogenes surface molecule that facilitates liver colonization. However, the involvement of gC1qR-p33 in L. monocytogenes–platelet association has not been described, and our data demonstrated that L. monocytogenes–platelet binding in vivo was dominated by a C3-mediated mechanism. Our data also preclude the possibility of involvement of immunoglobulins or C5, whose binding to S. aureus or Streptococcus sanguis promotes in vitro platelet aggregation via a mechanism involving the platelet Fc receptor and complement fixation20,34. This mechanism, termed 'slow activation' to distinguish it from two complement-independent mechanisms of 'rapid' in vitro platelet activation32, requires 7–19 min for S. sanguis34. In contrast, our in vivo experiments indicated that complement-mediated platelet association with L. monocytogenes also occurred without immunoglobulins (Rag1−/− mice) or C5 and within a time frame as short as 1 min. The dispensability of immunoglobulins also precludes the possibility of involvement of classical complement activation, as we confirmed in C4b−/− and C1qa−/− mice.
A longstanding question has been what platelet receptor is responsible for C3-mediated platelet adhesion. In contrast to human platelets, for which true complement receptor expression has been described35,36, such a receptor has been elusive on mouse platelets. However, mouse platelets express and bind complement regulatory proteins that can interact with C3 fragments to protect themselves from complement-mediated damage37,38. We found that GPIb, a leucine-rich glycoprotein receptor not previously associated with complement biology, had a critical role in the association of complement C3–opsonized bacteria with platelets. This is a previously unidentified role for this receptor, which is uniquely expressed on platelets and platelet-forming megakaryocytes.
In conclusion, we have identified a complement C3– and platelet GPIb–based shuttling mechanism for endovascular bacteria to CD8α+ DCs in the spleen. This mechanism balances rapid clearance and destruction of blood-borne pathogens through the reticuloendothelial system with the induction of adaptive immune responses. As DCs have broad relevance to immunity and tolerance, we suggest that the complement- and platelet-dependent targeting mechanism we identified here may be a factor to consider in vaccination strategies39, cross-presentation40, removal of apoptotic cells and tolerance41.
Methods
Mice.
C1qa−/− mice42, C3−/− mice25, C3ar1−/− mice43, C4b−/− mice44, C5mut/mut GP1ba−/− mice23, Rag1−/− mice45, CD11c-DTR transgenic mice8, OT-1 mice (transgenic expression of a TCR –specific for ovalbumin peptide, amino acids 257–264)46 carrying the congenic CD90.1+ marker and wild-type mice, all on C57BL/6 genetic background, except C5mut/mut (A/J), were derived by in-house breeding under specific pathogen–free conditions at the University of Zurich and Technische Universität München. Experiments were carried out according to the respective local veterinary laws and institutional guidelines.
Bacteria and infections.
Bacteria were grown to exponential phase at 37 °C in BHI broth and washed; inoculums were prepared in PBS. L. monocytogenes wild-type strain 10403S was administered intravenously at a dose of 0.5 × 104 to 1 × 104 colony-forming units (CFU) to determine spleen burdens at 1, 3 and 7 d after infection, 1 × 108 CFU for early clearance kinetic studies. For experiments involving splenic cell sorting, mice were infected intravenously with 0.5 × 106 to 1 × 106 CFU L. monocytogenes (strain 10403S) and spleens were collected after 1 h. For analysis of CD8+ T cell responses at day 7, 1 × 104 CFU ΔActA-L. monocytogenes–ovalbumin47 or 1 × 108 plaque-forming units of ovalbumin-expressing modified vaccinia virus Ankara48 were administered intravenously. Fluorescent traceable bacteria were obtained by incubation for 30 min at 37 °C in PBS containing 5 μM CSFE (carboxyfluorescein diacetate succinimidyl ester) at a density of 1 × 109 CFU per ml. For analysis of in vivo platelet binding, CFSE-labeled L. monocytogenes (10403S), S. aureus (Leibniz Institute German Collection of Microorganisms and Cell Cultures (DSMZ) 20231), E. fecalis (DMSZ 20478), B. subtilis (DSMZ 10) or S. pneumoniae (encapsulated strain D39/serotype 2, and its noncapsular R6 derivative) was used. In vitro infection of fresh peripheral blood for blocking studies was done in the presence of 50 μg lepirudin (Refludan), 10 μg antibody (antibody to GPIa-IIa (anti-GPIa-IIa; 23C11), anti- GPIbβ (p0p2), anti-GPIbα (p0p/B), anti-P-selectin (5C8), anti-LFA-1 (15G9), anti-PECAM1 (KIR1), anti-GPV (DOM1), anti-GPIIbIIIa (JON/A) and anti-GPVI (JAQ2)) and 1 × 108 CFU CFSE-labeled L. monocytogenes per milliliter blood, added in that order. In some experiments, L. monocytogenes were preopsonized with complement by mixture of equal volumes of fresh wild-type mouse serum (or C3−/− control serum) and washed bacteria (1 × 109 CFU/ml). After 30 min of incubation at 37 °C, bacteria were washed repeatedly in PBS. The C3 content of serum, wash supernatants and opsonized bacteria was determined by ELISA as described49. Bacterial titers of blood aliquots, homogenized organs, sorted cells and inoculums were determined by plating on BHI agar.
Complement, platelet, DC and phagocyte depletions.
Transient in vivo depletion of C3 was achieved with intraperitoneal injection with 25 μg CVF (Quidel) at the appropriate time points and verified by ELISA as described49. Mice were depleted of platelets by single intravenous injection of anti-CD42b (4 μg per gram body weight) according to the manufacturer's instruction (Emfret Analytics), and their absence was verified by flow cytometry staining with anti-CD41 (MWReg30 BD Biosciences) in peripheral blood. CD11c-DTR transgenic mice were depleted of DCs with diphtheria toxin (4 ng per gram body weight, injected intraperitoneally; Sigma). Depletion of phagocytes of the reticuloendothelial system was achieved by systemic application of clodronate liposomes, prepared and administered as described50. Depletion of DCs and phagocytes was verified by histological analysis of liver and spleen as described14.
Analysis of platelets.
Blood was immediately diluted 20-fold in flow cytometry buffer (PBS, 0.5% (wt/vol) BSA) containing heparin (50 IU/ml) for inhibition of ex vivo clotting, platelet aggregation and complement activation. Samples were kept at 20 °C and manipulated minimally; platelet-specific anti-CD41 (MWReg30; BD Biosciences) was titrated and added directly to the sample, followed by dilution of the sample 1:10 in flow cytometry buffer. Samples were then acquired on a FACSCalibur (BD Biosciences) and analyzed with FlowJo software (TreeStar). Alternatively, a sample aliquot was photographed with a DMRB fluorescence microscope (Leica) connected to an AxioCam MRc camera with Axiovision software (Zeiss).
Analysis of L. monocytogenes–infected splenocytes.
Cells were analyzed described14; spleens were removed and digested with collagenase for isolation of splenocytes at 1 h after intravenous infection with L. monocytogenes. After being washed in gentamicin-containing medium (5 μg/ml) to prevent extracellular growth of L. monocytogenes, cells were preincubated with anti-CD16-CD32 (2.4G2; BD Biosciences) and were subsequently stained with anti-CD8a (5H10; Caltag), anti-CD11c (HL3), anti-CD11b (M1/70) and anti-Ly6G (1Ab; all from BD Biosciences). Propidium iodide (Molecular Probes) was used for the discrimination of live or dead cells before sorting or was omitted for intracellular staining (Fixation/Permeabilization buffer, eBioscience) with anti-CD41 (MWReg30; BD Biosciences). Cell populations were sorted into pure FCS on a MoFlo Legacy flow cytometer (Beckman Coulter); their purity (>95%) was verified on a CyAn ADP Lx (Beckman Coulter) and they were lysed with Triton-X and plated on BHI plates for quantification of bacteria.
Analysis of CD8+ T cell responses.
Ovalbumin-specific cytotoxic T cell responses to infection with ΔActA-L. monocytogenes–ovalbumin were analyzed among endogenous and adoptively transferred OT-I CD8+ T cells (CD90.1+). At 1 d before infection, 100 naive (CD44loCD8+) live (propidium iodide–negative) OT-I cells were sorted from peripheral blood of OT-I (CD90.1+) mice on a MoFlo Legacy flow cytometer (Beckman Coulter) and were transferred intraperitoneally into recipient mice (CD90.2+). Splenocytes were analyzed 1 week after infection on a CyAn ADP Lx (Beckman Coulter). Ovalbumin-specific cytotoxic T cells were detected by flow cytometry with anti-CD3 (17A2; BD Biosciences) and anti-CD8 (5H10; Invitrogen), in combination with H2-Kb–SIINFEKL multimer for endogenous cells or anti-CD90.1 (OX-7; BD Biosciences) for transferred OT-I cells.
References
Savina, A. & Amigorena, S. Phagocytosis and antigen presentation in dendritic cells. Immunol. Rev. 219, 143–156 (2007).
van Lookeren Campagne, M., Wiesmann, C. & Brown, E.J. Macrophage complement receptors and pathogen clearance. Cell. Microbiol. 9, 2095–2102 (2007).
Ochsenbein, A.F. et al. Control of early viral and bacterial distribution and disease by natural antibodies. Science 286, 2156–2159 (1999).
Mebius, R.E. & Kraal, G. Structure and function of the spleen. Nat. Rev. Immunol. 5, 606–616 (2005).
Idoyaga, J., Suda, N., Suda, K., Park, C.G. & Steinman, R.M. Antibody to Langerin/CD207 localizes large numbers of CD8α+ dendritic cells to the marginal zone of mouse spleen. Proc. Natl. Acad. Sci. USA 106, 1524–1529 (2009).
Backer, R. et al. Effective collaboration between marginal metallophilic macrophages and CD8+ dendritic cells in the generation of cytotoxic T cells. Proc. Natl. Acad. Sci. USA 107, 216–221 (2010).
Pamer, E.G. Immune responses to Listeria monocytogenes. Nat. Rev. Immunol. 4, 812–823 (2004).
Jung, S. et al. In vivo depletion of CD11c+ dendritic cells abrogates priming of CD8+ T cells by exogenous cell-associated antigens. Immunity 17, 211–220 (2002).
Reinicke, A.T., Omilusik, K.D., Basha, G. & Jefferies, W.A. Dendritic cell cross-priming is essential for immune responses to Listeria monocytogenes. PLoS ONE 4, e7210 (2009).
Zammit, D.J., Cauley, L.S., Pham, Q.M. & Lefrancois, L. Dendritic cells maximize the memory CD8 T cell response to infection. Immunity 22, 561–570 (2005).
Stemberger, C. et al. A single naive CD8+ T cell precursor can develop into diverse effector and memory subsets. Immunity 27, 985–997 (2007).
Belz, G.T., Shortman, K., Bevan, M.J. & Heath, W.R. CD8α+ dendritic cells selectively present MHC class I-restricted noncytolytic viral and intracellular bacterial antigens in vivo. J. Immunol. 175, 196–200 (2005).
Aoshi, T. et al. The cellular niche of Listeria monocytogenes infection changes rapidly in the spleen. Eur. J. Immunol. 39, 417–425 (2009).
Neuenhahn, M. et al. CD8α+ dendritic cells are required for efficient entry of Listeria monocytogenes into the spleen. Immunity 25, 619–630 (2006).
Aichele, P. et al. Macrophages of the splenic marginal zone are essential for trapping of blood-borne particulate antigen but dispensable for induction of specific T cell responses. J. Immunol. 171, 1148–1155 (2003).
Skamene, E. & Chayasirisobhon, W. Enhanced resistance to Listeria monocytogenes in splenectomized mice. Immunology 33, 851–858 (1977).
Neuenhahn, M., Schiemann, M. & Busch, D.H. DCs in mouse models of intracellular bacterial infection. Methods Mol. Biol. 595, 319–329 (2010).
Croize, J., Arvieux, J., Berche, P. & Colomb, M.G. Activation of the human complement alternative pathway by Listeria monocytogenes: evidence for direct binding and proteolysis of the C3 component on bacteria. Infect. Immun. 61, 5134–5139 (1993).
Ford, I. & Douglas, C.W. The role of platelets in infective endocarditis. Platelets 8, 285–294 (1997).
Loughman, A. et al. Roles for fibrinogen, immunoglobulin and complement in platelet activation promoted by Staphylococcus aureus clumping factor A. Mol. Microbiol. 57, 804–818 (2005).
Nguyen, T., Ghebrehiwet, B. & Peerschke, E.I. Staphylococcus aureus protein A recognizes platelet gC1qR/p33: a novel mechanism for staphylococcal interactions with platelets. Infect. Immun. 68, 2061–2068 (2000).
Kleinschnitz, C. et al. Targeting platelets in acute experimental stroke: impact of glycoprotein Ib, VI, and IIb/IIIa blockade on infarct size, functional outcome, and intracranial bleeding. Circulation 115, 2323–2330 (2007).
Kanaji, T., Russell, S. & Ware, J. Amelioration of the macrothrombocytopenia associated with the murine Bernard-Soulier syndrome. Blood 100, 2102–2107 (2002).
Cunnion, K.M., Benjamin, D.K. Jr., Hester, C.G. & Frank, M.M. Role of complement receptors 1 and 2 (CD35 and CD21), C3, C4, and C5 in survival by mice of Staphylococcus aureus bacteremia. J. Lab. Clin. Med. 143, 358–365 (2004).
Wessels, M.R. et al. Studies of group B streptococcal infection in mice deficient in complement component C3 or C4 demonstrate an essential role for complement in both innate and acquired immunity. Proc. Natl. Acad. Sci. USA 92, 11490–11494 (1995).
Hyams, C., Camberlein, E., Cohen, J.M., Bax, K. & Brown, J.S. The Streptococcus pneumoniae capsule inhibits complement activity and neutrophil phagocytosis by multiple mechanisms. Infect. Immun. 78, 704–715 (2010).
Figueroa, J.E. & Densen, P. Infectious diseases associated with complement deficiencies. Clin. Microbiol. Rev. 4, 359–395 (1991).
Drevets, D.A. & Campbell, P.A. Roles of complement and complement receptor type 3 in phagocytosis of Listeria monocytogenes by inflammatory mouse peritoneal macrophages. Infect. Immun. 59, 2645–2652 (1991).
Nakayama, Y. et al. C3 promotes expansion of CD8+ and CD4+ T cells in a Listeria monocytogenes infection. J. Immunol. 183, 2921–2931 (2009).
Gregory, S.H. et al. Complementary adhesion molecules promote neutrophil-Kupffer cell interaction and the elimination of bacteria taken up by the liver. J. Immunol. 168, 308–315 (2002).
Helmy, K.Y. et al. CRIg: a macrophage complement receptor required for phagocytosis of circulating pathogens. Cell 124, 915–927 (2006).
Fitzgerald, J.R., Foster, T.J. & Cox, D. The interaction of bacterial pathogens with platelets. Nat. Rev. Microbiol. 4, 445–457 (2006).
Braun, L., Ghebrehiwet, B. & Cossart, P. gC1q-R/p32, a C1q-binding protein, is a receptor for the InlB invasion protein of Listeria monocytogenes. EMBO J. 19, 1458–1466 (2000).
Ford, I. et al. The role of immunoglobulin G and fibrinogen in platelet aggregation by Streptococcus sanguis. Br. J. Haematol. 97, 737–746 (1997).
Cosgrove, L.J., d'Apice, A.J., Haddad, A., Pedersen, J. & McKenzie, I.F. CR3 receptor on platelets and its role in the prostaglandin metabolic pathway. Immunol. Cell Biol. 65, 453–460 (1987).
Vik, D.P. & Fearon, D.T. Cellular distribution of complement receptor type 4 (CR4): expression on human platelets. J. Immunol. 138, 254–258 (1987).
Kim, D.D. et al. Deficiency of decay-accelerating factor and complement receptor 1-related gene/protein y on murine platelets leads to complement-dependent clearance by the macrophage phagocytic receptor CRIg. Blood 112, 1109–1119 (2008).
Alexander, J.J., Hack, B.K., Cunningham, P.N. & Quigg, R.J. A protein with characteristics of factor H is present on rodent platelets and functions as the immune adherence receptor. J. Biol. Chem. 276, 32129–32135 (2001).
Mollenkopf, H., Dietrich, G. & Kaufmann, S.H. Intracellular bacteria as targets and carriers for vaccination. Biol. Chem. 382, 521–532 (2001).
Heath, W.R. et al. Cross-presentation, dendritic cell subsets, and the generation of immunity to cellular antigens. Immunol. Rev. 199, 9–26 (2004).
Qiu, C.H. et al. Novel subset of CD8α+ dendritic cells localized in the marginal zone is responsible for tolerance to cell-associated antigens. J. Immunol. 182, 4127–4136 (2009).
Botto, M. et al. Homozygous C1q deficiency causes glomerulonephritis associated with multiple apoptotic bodies. Nat. Genet. 19, 56–59 (1998).
Humbles, A.A. et al. A role for the C3a anaphylatoxin receptor in the effector phase of asthma. Nature 406, 998–1001 (2000).
Fischer, M.B. et al. Regulation of the B cell response to T-dependent antigens by classical pathway complement. J. Immunol. 157, 549–556 (1996).
Mombaerts, P. et al. RAG-1-deficient mice have no mature B and T lymphocytes. Cell 68, 869–877 (1992).
Hogquist, K.A. et al. T cell receptor antagonist peptides induce positive selection. Cell 76, 17–27 (1994).
Bahjat, K.S. et al. Cytosolic entry controls CD8+-T-cell potency during bacterial infection. Infect. Immun. 74, 6387–6397 (2006).
Staib, C., Drexler, I. & Sutter, G. Construction and isolation of recombinant MVA. Methods Mol. Biol. 269, 77–100 (2004).
Verschoor, A., Brockman, M.A., Knipe, D.M. & Carroll, M.C. Cutting edge: myeloid complement C3 enhances the humoral response to peripheral viral infection. J. Immunol. 167, 2446–2451 (2001).
Van Rooijen, N. & Sanders, A. Liposome mediated depletion of macrophages: mechanism of action, preparation of liposomes and applications. J. Immunol. Methods 174, 83–93 (1994).
Acknowledgements
We thank S. Gordon, P. Lachmann and H. Wagner for input; M. Botto (Imperial College, London) for C1qa−/− mice; M. Carroll (Harvard Medical School) for C3−/− and C4b−/− mice; C. Gerard (Harvard Medical School) for C3ar−/− mice; F. Petry (Johannes Gutenberg University of Mainz, Germany) for C1qa−/− mice; M. van der Linden (University Hospital Aachen, Germany) for Streptococcus strains; S. Feihl and V. Greifenberg for bacterial typing; L. Henkel, M. Schiemann and K. Wild for flow cytometry cell sorting; K. Mink, S. Vieweg and A. Wanisch for experimental assistance; and L. Layland for support preparing the manuscript. Supported by the German Research Foundation SFB 914 (TP-B4 to A.V. and D.H.B.) and SFB 576 (TP-A8 to D.H.B.), the Swiss National Foundation (3100AO-100779/2 and 3100AO-100068/2 to H.H. and R.M.Z.), the German Center for Infection Research (DZIF; D.H.B.) and the European Commission (Marie Curie Fellowship to A.V.).
Author information
Authors and Affiliations
Contributions
A.V., M.N., A.A.N., A.P., A.S. and P.G. did experiments; B.N. and S.M. supplied reagents and assisted with data interpretation; A.V. and D.H.B. conceived the study; A.V., M.N., A.A.N. and P.G. analyzed the data; A.V., H.H., R.M.Z. and D.H.B. planned the experiments and supervised the study. A.V. and D.H.B. wrote the paper.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–2 (PDF 251 kb)
Rights and permissions
About this article
Cite this article
Verschoor, A., Neuenhahn, M., Navarini, A. et al. A platelet-mediated system for shuttling blood-borne bacteria to CD8α+ dendritic cells depends on glycoprotein GPIb and complement C3. Nat Immunol 12, 1194–1201 (2011). https://doi.org/10.1038/ni.2140
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ni.2140
This article is cited by
-
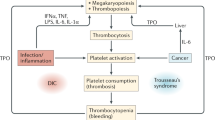
The GPIb-IX complex on platelets: insight into its novel physiological functions affecting immune surveillance, hepatic thrombopoietin generation, platelet clearance and its relevance for cancer development and metastasis
Experimental Hematology & Oncology (2022)
-
Interplay between inflammation and thrombosis in cardiovascular pathology
Nature Reviews Cardiology (2021)
-
Patrolling the vascular borders: platelets in immunity to infection and cancer
Nature Reviews Immunology (2019)
-
The inflammatory effects of TNF-α and complement component 3 on coagulation
Scientific Reports (2018)
-
Regulator-dependent mechanisms of C3b processing by factor I allow differentiation of immune responses
Nature Structural & Molecular Biology (2017)