Abstract
Purpose
Patients with a body mass index (BMI) ≥30 kg/m2 experience more severe atelectasis following cardiac surgery than those with normal BMI and its resolution is slower. This study aimed to compare extubation of patients post-cardiac surgery with a BMI ≥30 kg/m2 onto high-flow nasal cannulae (HFNC) with standard care to determine whether HFNC could assist in minimising post-operative atelectasis and improve respiratory function.
Methods
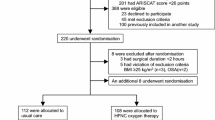
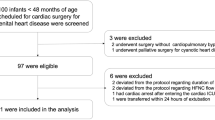
In this randomised controlled trial, patients received HFNC or standard oxygen therapy post-extubation. The primary outcome was atelectasis on chest X-ray. Secondary outcomes included oxygenation, respiratory rate (RR), subjective dyspnoea, and failure of allocated treatment.
Results
One hundred and fifty-five patients were randomised, 74 to control, 81 to HFNC. No difference was seen between groups in atelectasis scores on Days 1 or 5 (median scores = 2, p = 0.70 and p = 0.15, respectively). In the 24-h post-extubation, there was no difference in mean PaO2/FiO2 ratio (HFNC 227.9, control 253.3, p = 0.08), or RR (HFNC 17.2, control 16.7, p = 0.17). However, low dyspnoea levels were observed in each group at 8 h post-extubation, median (IQR) scores were 0 (0–1) for control and 1 (0–3) for HFNC (p = 0.008). Five patients failed allocated treatment in the control group compared with three in the treatment group [Odds ratio 0.53, (95 % CI 0.11, 2.24), p = 0.40].
Conclusions
In this study, prophylactic extubation onto HFNC post-cardiac surgery in patients with a BMI ≥30 kg/m2 did not lead to improvements in respiratory function. Larger studies assessing the role of HFNC in preventing worsening of respiratory function and intubation are required.




Similar content being viewed by others
References
O’Driscoll BR, Howard LS, Davison AG (2008) BTS guideline for emergency oxygen use in adult patients. Thorax 63:1–68
Xue FS, Li BW, Zhang GS, Liao X, Zhang YM, Liu JH, An G, Luo LK (1999) The influence of surgical sites on early postoperative hypoxemia in adults undergoing elective surgery. Anesth Analg 88:213–219
Joshi J, Fraser JF, Mullany DV (2005) The high risk cardiac surgical patient. Curr Anaesth Crit Care 16:369–383
Zarbock A, Mueller E, Netzer S, Gabriel A, Feindt P, Kindgen-Milles D (2009) Prophylactic nasal continuous positive airway pressure following cardiac surgery protects from postoperative pulmonary complications: a prospective, randomized, controlled trial in 500 patients. Chest 135:1252–1259
Pelosi P, Ravagnan I, Giurati G, Panigada M, Bottino N, Tredici S, Eccher G, Gattinoni L (1999) Positive end-expiratory pressure improves respiratory function in obese but not in normal subjects during anesthesia and paralysis. Anesthesiology 91:1221–1231
Eichenberger A, Proietti S, Wicky S, Frascarolo P, Suter M, Spahn DR, Magnusson L (2002) Morbid obesity and postoperative pulmonary atelectasis: an underestimated problem. Anesth Analg 95:1788–1792
World Health Organisation(2014) Obesity and overweight. http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed 29 Sept 2014
Wynne R, Botti M (2004) Postoperative pulmonary dysfunction in adults after cardiac surgery with cardiopulmonary bypass: clinical significance and implications for practice. Am J Crit Care 13:384–393
Tenling A, Hachenberg T, Tyden H, Wegenius G, Hedenstierna G (1998) Atelectasis and gas exchange after cardiac surgery. Anesthesiology 89:371–378
Lumb AB, Greenhill SJ, Simpson MP, Stewart J (2010) Lung recruitment and positive airway pressure before extubation does not improve oxygenation in the post-anaesthesia care unit: a randomized clinical trial. Br J Anaesth 104:643–647
Al Jaaly E, Fiorentino F, Reeves BC, Ind PW, Angelini GD, Kemp S, Shiner RJ (2013) Effect of adding postoperative noninvasive ventilation to usual care to prevent pulmonary complications in patients undergoing coronary artery bypass grafting: a randomized controlled trial. J Thorac Cardiovasc Surg 146:912–918
Celebi S, Koner O, Menda F, Omay O, Gunay I, Suzer K, Cakar N (2008) Pulmonary effects of noninvasive ventilation combined with the recruitment maneuver after cardiac surgery. Anesth Analg 107:614–619
Pinilla JC, Oleniuk FH, Tan L, Rebeyka I, Tanna N, Wilkinson A, Bharadwaj B (1990) Use of a nasal continuous positive airway pressure mask in the treatment of postoperative atelectasis in aortocoronary bypass surgery. Crit Care Med 18:836–840
Gregoretti C, Confalonieri M, Navalesi P, Squadrone V, Frigerio P, Beltrame F, Carbone G, Conti G, Gamna F, Nava S, Calderini E, Skrobik Y, Antonelli M (2002) Evaluation of patient skin breakdown and comfort with a new face mask for non-invasive ventilation: a multi-center study. Intensive Care Med 28:278–284
Lee JH, Rehder KJ, Williford L, Cheifetz IM, Turner DA (2013) Use of high flow nasal cannula in critically ill infants, children, and adults: a critical review of the literature. Intensive Care Med 39:247–257
Schibler A, Pham TM, Dunster KR, Foster K, Barlow A, Gibbons K, Hough JL (2011) Reduced intubation rates for infants after introduction of high-flow nasal prong oxygen delivery. Intensive Care Med 37:847–852
Woodhead DD, Lambert DK, Clark JM, Christensen RD (2006) Comparing two methods of delivering high-flow gas therapy by nasal cannula following endotracheal extubation: a prospective, randomized, masked, crossover trial. J Perinatol 26:481–485
Corley A, Caruana LR, Barnett AG, Tronstad O, Fraser JF (2011) Oxygen delivery through high-flow nasal cannulae increase end-expiratory lung volume and reduce respiratory rate in post-cardiac surgical patients. Br J Anaesth 107:998–1004
Parke R, McGuinness S, Eccleston M (2009) Nasal high-flow therapy delivers low level positive airway pressure. Br J Anaesth 103:886–890
Sztrymf B, Messika J, Bertrand F, Hurel D, Leon R, Dreyfuss D, Ricard JD (2011) Beneficial effects of humidified high flow nasal oxygen in critical care patients: a prospective pilot study. Intensive Care Med 37:1780–1786
Sztrymf B, Messika J, Mayot T, Lenglet H, Dreyfuss D, Ricard JD (2012) Impact of high-flow nasal cannula oxygen therapy on intensive care unit patients with acute respiratory failure: a prospective observational study. J Crit Care 27:324
Maggiore SM, Idone FA, Vaschetto R, Festa R, Cataldo A, Antonicelli F, Montini L, De Gaetano A, Navalesi P, Antonelli M (2014) Nasal high-flow versus Venturi mask oxygen therapy after extubation. Effects on oxygenation, comfort, and clinical outcome. Am J Respir Crit Care Med 190:282–288
Itagaki T, Okuda N, Tsunano Y, Kohata H, Nakataki E, Onodera M, Imanaka H, Nishimura M (2014) Effect of high-flow nasal cannula on thoraco-abdominal synchrony in adult critically ill patients. Respir Care 59:70–74
Rittayamai N, Tscheikuna J, Rujiwit P (2014) High-flow nasal cannula versus conventional oxygen therapy after endotracheal extubation: a randomized crossover physiologic study. Respir Care 59:485–490
Roca O, Riera J, Torres F, Masclans JR (2010) High-flow oxygen therapy in acute respiratory failure. Respir Care 55:408–413
Schwabbauer N, Berg B, Blumenstock G, Haap M, Hetzel J, Riessen R (2014) Nasal high-flow oxygen therapy in patients with hypoxic respiratory failure: effect on functional and subjective respiratory parameters compared to conventional oxygen therapy and non-invasive ventilation (NIV). BMC Anesth 14:66
Dysart K, Miller TL, Wolfson MR, Shaffer TH (2009) Research in high flow therapy: mechanisms of action. Respir Med 103:1400–1405
Ricard JD (2012) High flow nasal oxygen in acute respiratory failure. Minerva Anestesiol 78:836–841
Richter Larsen K, Ingwersen U, Thode S, Jakobsen S (1995) Mask physiotherapy in patients after heart surgery: a controlled study. Intensive Care Med 21:469–474
Bozbas SS, Dedekarginoglu BE, Cakir S, Karakayali FY, Eyuboglu FO (2012) Effects of use of Boussignac CPAP on development of post-operative atelectasis. Euro Resp J 40:2060
Pasquina P, Merlani P, Granier JM, Ricou B (2004) Continuous positive airway pressure versus noninvasive pressure support ventilation to treat atelectasis after cardiac surgery. Anesth Analg 99:1001–1008
Treschan TA, Kaisers W, Schaefer MS, Bastin B, Schmalz U, Wania V, Eisenberger CF, Saleh A, Weiss M, Schmitz A, Kienbaum P, Sessler DI, Pannen B, Beiderlinden M (2012) Ventilation with low tidal volumes during upper abdominal surgery does not improve postoperative lung function. Br J Anaesth 109:263–271
Pierce LNB (2007) Management of the mechanically ventilated patient. Saunders Elsevier, St Louis
American Thoracic Society (2002) ATS statement: guideline for the 6 minute walk test. Am J Resp Crit Care Med 166:111–117
Parke R, McGuinness S, Dixon R, Jull A (2013) Open-label, phase II study of routine high-flow nasal oxygen therapy in cardiac surgical patients. Br J Anaesth 111:925–931
Parke RL, Eccleston ML, McGuinness SP (2011) The effects of flow on airway pressure during nasal high-flow oxygen therapy. Respir Care 56:1151–1155
Parke RL, McGuinness SP, Eccleston ML (2011) A preliminary randomized controlled trial to assess effectiveness of nasal high-flow oxygen in intensive care patients. Respir Care 56:265–270
Calfee CS, Eisner MD, Ware LB, Thompson BT, Parsons PE, Wheeler AP, Korpak A, Matthay MA (2007) Trauma-associated lung injury differs clinically and biologically from acute lung injury due to other clinical disorders. Crit Care Med 35:2243–2250
Rothaar RC, Epstein SK (2003) Extubation failure: magnitude of the problem, impact on outcomes, and prevention. Curr Opin Crit Care 9:59–66
Acknowledgments
We would like to thank Drs Rachael O’Rourke and Johnny Ayres for scoring the chest X-rays. We would also like to gratefully acknowledge the assistance and enthusiasm of the ICU staff, without whom this study would not have been possible. Prof Fraser acknowledges support through his Health Research Fellowship from the Office of Health and Medical Research, Queensland Health.
Conflicts of interest
John F. Fraser has received an unrestricted grant from Fisher and Paykel Healthcare Ltd in support of the current study totalling NZ$50 000. Fisher and Paykel Healthcare Ltd had no part in study design, data collection, data analysis, or creation of the manuscript. John F. Fraser has received assistance from Fisher and Paykel Healthcare Ltd to support travel and accommodation costs to attend research meetings totalling approximately NZ$15.000; Amanda Corley has received assistance from Fisher and Paykel Healthcare Ltd to support travel and accommodation costs to attend two research meetings totalling NZ$3000. Authors Taressa Bull, Amy J. Spooner and Adrian G. Barnett declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Take-home message: In this randomised controlled trial, direct extubation onto high-flow nasal cannulae (HFNC) was not found to improve respiratory function after cardiac surgery in patients with a BMI ≥30 kg/m2 when compared with standard oxygen therapy.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Corley, A., Bull, T., Spooner, A.J. et al. Direct extubation onto high-flow nasal cannulae post-cardiac surgery versus standard treatment in patients with a BMI ≥30: a randomised controlled trial. Intensive Care Med 41, 887–894 (2015). https://doi.org/10.1007/s00134-015-3765-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-015-3765-6