Abstract
Purpose
The Berlin definition for acute respiratory distress syndrome (ARDS) is a new proposal for changing the American-European consensus definition but has not been assessed prospectively as yet. In the present study, we aimed to determine (1) the prevalence and incidence of ARDS with both definitions, and (2) the initial characteristics of patients with ARDS and 28-day mortality with the Berlin definition.
Methods
We performed a 6-month prospective observational study in the ten adult ICUs affiliated to the Public University Hospital in Lyon, France, from March to September 2012. Patients under invasive or noninvasive mechanical ventilation, with PaO2/FiO2 <300 mmHg regardless of the positive end-expiratory pressure (PEEP) level, and acute onset of new or increased bilateral infiltrates or opacities on chest X-ray were screened from ICU admission up to discharge. Patients with cardiogenic pulmonary edema were excluded. Patients were further classified into specific categories by using the American-European Consensus Conference and the Berlin definition criteria. The complete data set was measured at the time of inclusion. Patient outcome was measured at day 28 after inclusion.
Results
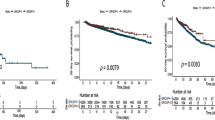
During the study period 3,504 patients were admitted and 278 fulfilled the American-European Consensus Conference criteria. Among them, 18 (6.5 %) did not comply with the Berlin criterion PEEP ≥ 5 cmH2O and 20 (7.2 %) had PaO2/FiO2 ratio ≤200 while on noninvasive ventilation. By using the Berlin definition in the remaining 240 patients (n = 42 mild, n = 123 moderate, n = 75 severe), the overall prevalence was 6.85 % and it was 1.20, 3.51, and 2.14 % for mild, moderate, and severe ARDS, respectively (P > 0.05 between the three groups). The incidence of ARDS amounted to 32 per 100,000 population per year, with values for mild, moderate, and severe ARDS of 5.6, 16.3, and 10 per 100,000 population per year, respectively (P < 0.05 between the three groups). The 28-day mortality was 35.0 %. It amounted to 30.9 % in mild, 27.9 % in moderate, and 49.3 % in severe categories (P < 0.01 between mild or moderate and severe, P = 0.70 between mild and moderate). In the Cox proportional hazard regression analysis ARDS stage was not significantly associated with patient death at day 28.
Conclusions
The present study did not validate the Berlin definition of ARDS. Neither the stratification by severity nor the PaO2/FiO2 at study entry was independently associated with mortality.
Similar content being viewed by others
Introduction
The American-European Consensus Conference (AECC) [1] definition of the acute lung injury (ALI)/acute respiratory distress syndrome (ARDS) has been used for many years for both academic and practical purposes. Over the years, however, several reports have challenged and criticized the AECC criteria for the diagnosis of ARDS. In particular, it was pointed out that the assessment of the oxygenation defect did not require standardized ventilator support [2–4]. The AECC definition has recently been revisited by an expert panel, which proposed some changes that led to the release of the Berlin definition [5]. The Berlin definition has produced new findings with the following being noteworthy: (1) acute onset was defined as occurring within 1 week after onset of new or worsened respiratory symptoms, (2) positive end-expiratory pressure (PEEP) of at least 5 cmH2O at the time of oxygenation assessment was mandated, (3) ARDS was stratified into three stages according to oxygenation severity at ARDS onset, (4) patients receiving continuous positive airway pressure/noninvasive ventilation may be included in the mild stage only. The term ALI was discarded and replaced by “mild” ARDS. Furthermore, on the basis of the data previously published in the field of evidence-based medicine, the experts summarized the strategies to be applied for ventilator and extraventilator treatments depending on the ARDS stage, separating these strategies into those which are proven and those which are not and therefore would require further studies [5]. The AECC and Berlin definition criteria were empirically evaluated by using retrospective cohorts [6]. However, the Berlin definition has not yet been evaluated prospectively in clinical situations. Therefore, the main purpose of the present study was to measure the prevalence and incidence of ARDS by using both the new and old ARDS criteria in the clinical field. The second aim was to describe the clinical characteristics and 28-day mortality of ARDS patients according to the three ARDS stages.
Methods
We designed a prospective observational study in the ten adult intensive care units (ICUs) of public hospitals affiliated to University of Lyon 1, France. The Lyon University health-care complex is based on three multidisciplinary hospitals and two specialized (one in cardiology and one in neurology) hospitals. Among the ten adult ICUs, there are three medical ICUs (one in each multidisciplinary hospital), four surgical ICUs, one burns ICU, and one medical-surgical ICU in each specialized hospital. All are open ICUs. Seven are run by anesthesiologists, two by medical intensivists, and one by a mixed medical team. Each ICU agreed to participate in the study. The protocol was approved by an ethics committee (Comité d’Ethique des Centres d’Investigation Clinique de l’Inter-région Rhône-Alpes-Auvergne, IRB number 5891, IRB file 2012-04). Informed consent from the patient or the next of kin was waived. The patients and/or their next of kin were approached and informed that they were included in this observational study. All the patients admitted to any of these ICUs were screened for eligibility up to their ICU discharge. Patients were included if they met the following inclusion criteria: age ≥18 years, invasive or noninvasive mechanical ventilation used for the ongoing acute respiratory failure, identified risk factor for ALI, ratio of arterial oxygen partial pressure to oxygen fraction in inspired gas (PaO2/FiO2) ≤300 mmHg regardless of PEEP level, and bilateral infiltrates or opacities on the chest X-ray. Patients were excluded if they had been previously admitted to any participating ICU for any reason from the onset of the present study. Patients with cardiogenic pulmonary edema as the main reason for the acute respiratory failure according to the clinician’s assessment were also excluded.
Protocol
Eligible patients were included when both oxygenation and chest-X-ray criteria were present simultaneously. The day of inclusion was the calendar day on which those criteria were present. The patients were followed up to ICU discharge. Data on patient outcome 28 days after inclusion was tracked. The decision to include the patient into the study and the decision for further adjudication into ARDS stages were taken prospectively by the clinicians in charge of the study in each ICU and checked by the research fellows afterwards. The protocol did not provide a set of general recommendations about ventilator (in particular with PEEP selection) and nonventilator (in particular with the use of neuromuscular blocking agents) management of patients with ALI/ARDS.
Data collection
The following data were recorded at ICU admission for the included patients: date of hospital and ICU admission, age, gender, origin, height, Simplified Acute Physiology Score (SAPS) II, and Charlson’s comorbidity score. The following data were recorded at the time of inclusion: invasive or noninvasive mechanical ventilation, cause of ALI, Sequential Organ Failure Assessment (SOFA) score (the worst value during the 24 h of the day of inclusion), AECC criteria, Berlin definition criteria, date of tracheal intubation if any, intravenous sedation, neuromuscular blocking agents, the worst PaO2/FiO2 ratio with the highest PEEP level available, ventilator settings, plateau pressure of the respiratory system and total PEEP recorded at the same time of the previously mentioned PaO2/FiO2 measurement, ventilator mode, heater-humidifier, heat and moisture exchanger, catheter mount. The major cause of death at ICU discharge was summarized from the final report for each patient into the following categories: multiple organ failure, refractory shock, cardiac arrest, hypoxemia, or other. In patients on noninvasive ventilation (NIV) who were intubated the measurements also included the worst PaO2/FiO2 ratio with the highest PEEP level available after intubation.
The study lasted from 26 March to 26 September 2012.
Data analysis
The quality control of the collected data was performed by research fellows at each center. We anonymized the personal data which were then entered into a database (Epi-data® software, freeware available at http://www.epidata.dk/links.htm) specifically developed for the study and registered with the Commission Nationale d’Informatique et des Libertés. The data analysis was performed by using Epi-Info 6.04 FR and SPSS softwares.
The following variables were computed: observed minute ventilation (=tidal volume × total respiratory frequency), theoretical minute ventilation (=observed minute ventilation + PaCO2/40 mmHg), static compliance of the respiratory system (=tidal volume/plateau pressure − total PEEP).
The prevalence of ARDS was computed as the ratio of the number of included ARDS patients to the number of patients screened during the study period.
The incidence of ARDS was expressed as the number of new ARDS cases per 100,000 population per year assuming 1,500,000 people living in Lyon during 2011 and was computed by censoring the length of follow-up to the ARDS occurrence. Therefore, the incidence was obtained as the number of included ARDS patients divided by the sum of the number of ICU days in both the screened patients and the ARDS patients and the number of ICU days without ARDS in those with ARDS.
The continuous data are presented as median (first–third quartile) and the categorical data in counts and percent of group. The data were compared by using the Chi-squared or Fisher’s exact test or ANOVA as appropriate. The incidence of ARDS was compared between the groups by using the Z score. The survival was assessed by using Kaplan–Meier graphs, which were compared by the log-rank test. A Cox proportional hazard regression model was constructed to control the impact of ARDS stage on 28-day mortality for confounding factors, specifically those variables of statistical significance by using the cutoff P < 0.10 for inclusion between survivors and nonsurvivors in the univariate comparison. We verified that the effect of these covariates was linear over time. Furthermore, owing to the expected high colinearity between the PaO2/FiO2 ratio and the three ARDS categories according the Berlin definition, we built two different Cox’s models, one with PaO2/FiO2 and one with ARDS categories as the independent covariates. The significant statistical threshold was set to P < 0.05.
Results
During this period, 3,504 patients were admitted to the 10 adult ICUs and 278 fulfilled eligibility criteria (Fig. 1). Among them, 18 (6.5 %) did not comply with the Berlin definition criterion of PEEP ≥ 5 cmH2O (Figs. 1, 2). Furthermore, 20 patients who received NIV alone could not be classified as moderate or severe ARDS according to the rules of the Berlin definition (Figs. 1, 2). These 38 patients were excluded from the further analysis using the Berlin definition, which was henceforth performed with 240 patients (Figs. 1, 2). One of them was lost to follow-up (Fig. 1). These 240 patients were split into mild (n = 42), moderate (n = 123), and severe (n = 75) categories according to the Berlin definition (Fig. 2).
Distribution of the 278 patients with acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) across the American-European Consensus Conference (AECC) and Berlin definition criteria depending on invasive or noninvasive mechanical ventilation. NIV noninvasive ventilation, PEEP positive end-expiratory pressure
The prevalence and incidence of ARDS according to the Berlin definition are displayed in Table 1. Moderate ARDS was the most frequent presentation of ARDS in this cohort. The characteristics of the patients in the three ARDS groups at ICU admission and at study inclusion are shown in Table 2. SOFA score was significantly higher in the severe ARDS category than in either the mild (P = 0.0285) or moderate (P = 0.0025) ARDS category. With the increased ARDS severity oxygenation worsened whilst PEEP and FiO2 increased significantly (Table 2). The measured and theoretical minute ventilation were not different between the ARDS groups, and hence the same was true for the proportion of patients with measured minute ventilation higher than 10 L min−1 (not shown). The plateau pressure was 21 (18–24), 21 (19–25), and 24 (21–27) cmH2O in the mild, moderate, and severe ARDS categories, respectively (P = 0.026). The corresponding values for the compliance of the respiratory system were 35 (30–48), 35 (29–45) and 38 (29–45) mL cmH2O−1, respectively (P = 0.87). There was no difference between the groups for the use of humidification strategies whilst the rate of use of catheter mount significantly decreased with ARDS severity (not shown). The rate of use of neuromuscular blockade at the time of inclusion increased with ARDS severity (Table 2). The risk factors for ARDS were similar across ARDS groups, with pneumonia as the primary cause, except for extrapulmonary sepsis whose occurrence decreased with ARDS severity (Table S1).
In the mild, moderate, and severe ARDS categories, the ICU length of stay was 10 (6–24), 14 (8–24), and 13 (6–22) days, respectively (P > 0.05). It was 11 (7–28), 15 (10–24), and 18 (11–32) days in survivors (P > 0.05) and 9 (5–19), 10 (4–24), and 8 (2–16) (P > 0.05) days in nonsurvivors at ICU discharge.
The 28-day mortality rate in the entire cohort of the 278 mechanically ventilated patients meeting the AECC criteria for ARDS and for ALI was 34.9 % and it was 35.1 % for the 240 patients meeting the Berlin criteria. In the mild, moderate, and severe ARDS categories, the 28-day mortality rate was 30.9 % (13/42), 27.9 % (34/122), and 49.3 % (37/75) (P = 0.008), respectively. The corresponding rates at ICU discharge were 35.7 % (15/42), 31.7 % (39/123), and 52 % (39/75) (P = 0.0176), respectively. The difference in 28-day and ICU discharge mortality rates was not significantly different between the mild and moderate groups. In the ALI and ARDS groups of the AECC definition, the mortality rates at ICU discharge and day 28 were 40.8 and 37.4 % (P = 0.387) and 36.7 and 34.5 % (P = 0.443), respectively. The cause of death at ICU discharge was not different across the three ARDS groups (P = 0.84, Table S2).
The cumulative probability of survival was significantly different across the three ARDS groups (Fig. 3). The univariate comparison between survivors and nonsurvivors and the results of the Cox proportional hazard regression model for 28-day mortality are shown in Tables S3 and 3, respectively. Neither the severity of ARDS by the Berlin definition nor the PaO2/FiO2 ratio was independently associated with mortality at day 28.
Discussion
We found that (1) 6.5 % of the patients with ALI/ARDS according to the AECC criteria could not be classified as ARDS from the Berlin definition, (2) the prevalence and incidence of ARDS were 6.85 % and 32 per 100,000 population per year, respectively, according to the Berlin definition, (3) the crude 28-day mortality rate was not different between the mild and moderate ARDS groups.
Defining ARDS is fundamental but is still a very controversial issue even after the recent Berlin definition proposal. Indeed, the modified ARDS definition by the Berlin task force has been criticized and challenged for different reasons, some of which are highlighted in the present study and discussed below. Of note, the proposal of the Berlin definition used a terminology similar to what others had previously suggested [7–10].
Methodology of present study
To the best of knowledge, this is the first study that prospectively assessed the Berlin definition of ARDS. According to its main goal, the present study had a specific design. Indeed, we checked every patient admitted to each of the participating ICUs for PaO2/FiO2 ratio and chest X-ray and included those who had PaO2/FiO2 ratio ≤300 mmHg regardless of PEEP level and infiltrates and/or opacities on the chest X-ray. We reasoned that once met simultaneously both aforementioned criteria should track all ARDS patients under both classification systems. Next, the patients were further classified according to the criteria pertaining to each definition system.
We found that 6.5 % of patients with ALI/ARDS according to the AECC definition could not be classified as having ARDS according to the Berlin definition because PEEP was less than 5 cmH2O. This finding was also reported when the panel empirically evaluated the Berlin definition [6]. The panel found that 12 % of patients with ALI/ARDS could not be classified by the Berlin definition criteria because data on PEEP were missing or PEEP was less than 5 cmH2O [6]. For the same reason, Costa and Amato [11] who meta-analyzed data of 1,752 patients included in six clinical trials [12–17] excluded 15 % of them [11]. These discrepant rates between the present study and the two others [6, 11] may be explained by the number of patients included and the prospective versus retrospective design. This observation should be kept in mind when designing further studies in ARDS using the Berlin definition and, hence potentially eligible patients must be checked with PEEP of at least 5 cmH2O. As suggested by previous reports [4, 18, 19], we think that it would be more appropriate to assess ARDS patients for clinical trials at a fixed, standardized level of PEEP and FiO2, within the first 12–24 h after study entry.
The issue of NIV
The Berlin definition acknowledged the use of NIV in ARDS. Therefore, patients receiving NIV or continuous positive airway pressure can be included as mild ARDS provided the other criteria for this category are met. This proposal matches the report of the increase in NIV use in the ICU worldwide from 5 % in 1998 to 14 % in 2010 [20]. This latter rate is quite similar to that of 16 % found in the “de novo” hypoxemic acute respiratory failure group in a recent survey done in France and in Belgium in 2,367 ICU patients over 2 months [21]. Apart from the 5 patients in our study who were under NIV at the time of inclusion and could be included as mild ARDS, 20 patients under NIV for ARDS should have been classified as moderate or severe ARDS according to the PaO2/FiO2 ratio. They were excluded from the present study because the Berlin definition specifically indicates that patients in these groups must be invasively ventilated. It is well known that PaO2/FiO2 values in patients under NIV or invasive mechanical ventilation are not comparable for several reasons: (1) lung volume is different in intubated and nonintubated patients, (2) functional residual capacity varies with the mode of ventilation because pleural pressure is different, (3) respiratory rate is different for the same PaO2, (4) tidal volume (VT) is different under NIV and invasive mechanical ventilation, (5) airway and transpulmonary pressures are not comparable in NIV vs. invasive mechanical ventilation.
In the retrospective empirical analysis for describing the Berlin modification of the AECC ARDS definition [6], 24 % of patients had a PaO2/FiO2 >200 mmHg at the time of enrollment (classified as non-ARDS or ALI by the AECC definition), introducing a bias because (1) in many centers these type of patients are usually not treated with invasive mechanical ventilation, and (2) as much as in 40 % of ARDS patients, PaO2/FiO2 increased above 200 mmHg when they are evaluated under standard ventilator settings [3].
Mortality
In the present study, overall 28-day mortality of patients categorized as mild ARDS was similar to those categorized as moderate ARDS (30.9 vs. 27.9 %). Furthermore, we found that the Berlin classification was not associated with 28-day mortality after adjusting for confounding factors. The results of the present study, if confirmed by others, should lead to a critical reappraisal of the Berlin proposal as discussed recently [18, 22]. The present result may be explained by the selection strategy of the PaO2/FiO2 ratio in our study to stratify the patients according to the Berlin definition, as we used the worst PaO2/FiO2 ratio at the highest PEEP. A similar finding was observed by Costa and Amato [11] even after adjustment for APACHE III, age, and pH when the oxygenation at baseline was taken into account. These observations raised the issue of the best timing relative to ICU admission in selecting the PaO2/FiO2. Indeed, when Costa and Amato [11] used the oxygenation taken 24 h later, the moderate ARDS patients had unadjusted and adjusted odds ratios (OR) for mortality of 1.65 and 1.49, respectively, which, even though relatively low, were significantly different from the mild ARDS taken as the reference (OR 1). By study design, our investigation missed the opportunity to evaluate the reassessment 24 h later. In a recent randomized controlled trial enrolling patients after a 12- to 24-h stabilization period, we found that the prone position was associated with a significant reduction in mortality as compared to the supine position [19]. However, the reassessment at 24 h also has potential bias and limitation. As an example, if at that time the patient has been placed in the prone position and oxygenation exhibits a substantial improvement, it would be hard to interpret the associated change in ARDS category.
It should also be noted that even appropriate baseline PEEP does not predict mortality [18, 23] baseline FiO2 does [18, 24]. In the present study, the clinicians used relatively low levels of PEEP in all three ARDS categories. However, the higher the ARDS severity the higher the PEEP used in the present study. As already mentioned and further discussed below, the protocol did not provide recommendations for ventilating ARDS patients, and hence the real-life practice was left to the attending clinician’s discretion. The optimal PEEP level and the way to reach this optimal level at the bedside are far from being defined. The individual meta-analysis by Briel et al. [25] found that higher PEEP was not associated with better hospital survival except, in the post hoc analysis, for patients with PaO2/FiO2 ≤ 200 mmHg. Furthermore, should higher PEEP be really beneficial to patient outcome, we are still left with the method to achieve this level. Indeed, each of three large randomized controlled trials [16, 26, 27] involved in this meta-analysis had a specific method to titrate PEEP and none of these was associated with improved survival.
The neuromuscular blocking agents use in our study was associated with worsened outcome in univariate comparison between survivors and nonsurvivors. This association was no longer significant after adjustment for confounding factors. Early and brief use of neuromuscular blocking agents has been found to be associated with better survival than placebo in severe ARDS [11]. It should be noted that a substantial rate of patients in the mild ARDS category in the present study did receive neuromuscular blocking agents. The reason for this is not clear.
We found that the patients in the mild ARDS category had similar mortality to that in the moderate category. This finding is consistent with the similar SAPS II and global SOFA score in both groups. The reason why SAPS II and SOFA were not lower in the mild than in the moderate ARDS is unclear. We observed that extrapulmonary ARDS tended to be more frequent in the former than in the latter category. It is unclear if this could impact on mortality. Similar explanations should pertain to the observation that patients with ALI had similar mortality as patients with ARDS.
Prevalence and incidence of ARDS
The moderate ARDS group had the highest prevalence and incidence in our cohort. This was also found in the validation cohort, in which the frequency of mild, moderate, and severe categories was 22, 50, and 28 %, respectively [6]. The overall incidence of ARDS in the present study was in-between that found in the USA [28] and Europe [7, 29, 30]. Differences in the inclusion periods, inclusion duration, definition of ARDS used, and accuracy in the denominator in the present study could explain the discrepant results. Other explanations are detailed in the next section.
Limitations and strengths
Our study had several limitations. First, the study design lacked a set of general recommendations for ventilating ARDS patients, and hence for ventilating, screening, enrolling, and assessing enrolled patients. However, such a design was a way to apply the Berlin proposal in real life. Second, the information about transient fall of PaO2/FiO2 as an exclusion criterion for enrolling patients was not recorded. Third, inclusion bias might have resulted from the plausible misclassification of patients with very light ALI as having mild or moderate ARDS due to an insufficient level of PEEP in their initial ventilator management and wrong inclusion of patients with a transient fall in the PaO2/FiO2 value resulting from patient–ventilator asynchronies, airway secretions, post-suctioning, sudden barotraumas, and hemodynamic instability. Fourth, the unexpected elevated mortality of patients with PaO2/FiO2 >200 was not clearly explained. Fifth, as patients were included in a non-epidemic time frame and contributing ICUs were part of a university hospital, the present results may be not generalizable to epidemic periods, like that which occurred with H1N1 infection [31], and to non-university ICUs. Sixth, covariates were measured at the time of inclusion and management afterwards was not recorded. Therefore, the multivariate analysis of mortality did not include variables that may impact on patient outcome, like prone positioning or fluid balance control [19]. A larger study involving more ICUs should be performed to address these issues. Since patients transferred from another ICU (who may not have yet had ARDS) were excluded there may have been an underestimate of ARDS prevalence. Finally, our cohort did not include patients without ARDS.
Our study had strengths as it was prospective, multicenter, the period of inclusion was short, which precluded any substantial change in either epidemiological factor or medical management, and the quality of the data was controlled. The study was conducted in a non-pandemic period. ICUs were medical, surgical, or both and would have covered a wide spectrum of the clinical situations at risk of developing ARDS.
The findings bring into question the ability of the Berlin definition to classify patients into three distinct groups with different mortality rates as proposed by the Berlin group.
In conclusion, the present study did not validate the Berlin definition of ARDS. Neither the stratification by severity nor the PaO2/FiO2 at study entry was independently associated with mortality.
References
Bernard GR, Artigas A, Brigham KL, The Consensus Committee et al (1994) Report of the American-European consensus conference on ARDS: definitions, mechanisms, relevant outcomes and clinical trial coordination. Intensive Care Med 20:225–232
Villar J, Perez-Mendez L, Kacmarek RM (1999) Current definitions of acute lung injury and the acute respiratory distress syndrome do not reflect their true severity and outcome. Intensive Care Med 25:930–935
Villar J, Perez-Mendez L, Lopez J et al (2007) An early PEEP/FiO2 trial identifies different degrees of lung injury in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med 176:795–804
Villar J, Kacmarek RM, Perez-Mendez L, Aguirre-Jaime A (2006) A high positive end-expiratory pressure, low tidal volume ventilatory strategy improves outcome in persistent acute respiratory distress syndrome: a randomized, controlled trial. Crit Care Med 34:1311–1318
Ferguson ND, Fan E, Camporota L et al (2012) The Berlin definition of ARDS: an expanded rationale, justification, and supplementary material. Intensive Care Med 38:1573–1582
Ranieri VM, Rubenfeld GD, Thompson BT et al (2012) Acute respiratory distress syndrome. The Berlin definition. JAMA 307:E1–E8
Villar J, Blanco J, Anon JM et al (2011) The ALIEN study: incidence and outcome of acute respiratory distress syndrome in the era of lung protective ventilation. Intensive Care Med 37:1932–1941
Villar J, Perez-Mendez L, Basaldua S et al (2011) A risk tertiles model for predicting mortality in patients with acute respiratory distress syndrome: age, plateau pressure, and P(aO(2))/F(IO(2)) at ARDS onset can predict mortality. Respir Care 56:420–428
Lopez-Fernandez Y, Azagra AM, de la Oliva P et al (2012) Pediatric acute lung injury epidemiology and natural history study: incidence and outcome of the acute respiratory distress syndrome in children. Crit Care Med 40:3238–3245
Villar J, Kacmarek RM (2013) What is new in refractory hypoxemia? Intensive Care Med 39:1207–1210
Costa EL, Amato MB (2013) The new definition for acute lung injury and acute respiratory distress syndrome: is there room for improvement? Curr Opin Crit Care 19:16–23
The Acute Respiratory Distress Syndrome Network, ARDSnet (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 342:1301–1308
Amato MB, Barbas CS, Medeiros DM et al (1998) Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med 338:347–354
Stewart TE, Meade MO, Cook DJ et al (1998) Evaluation of a ventilation strategy to prevent barotrauma in patients at high risk for acute respiratory distress syndrome. Pressure- and volume-limited ventilation strategy group. N Engl J Med 338:355–361
Brower RG, Shanholtz CB, Fessler HE et al (1999) Prospective, randomized, controlled clinical trial comparing traditional versus reduced tidal volume ventilation in acute respiratory distress syndrome patients. Crit Care Med 27:1492–1498
Brower RG, Lanken PN, MacIntyre N et al (2004) Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med 351:327–336
Brochard L, Roudot-Thoraval F, Roupie E et al (1998) Tidal volume reduction for prevention of ventilator-induced lung injury in acute respiratory distress syndrome. The multicenter trail group on tidal volume reduction in ARDS. Am J Respir Crit Care Med 158:1831–1838
Villar J, Perez-Mendez L, Blanco J et al (2013) A universal definition of ARDS: the PaO2/FiO2 ratio under a standard ventilatory setting—a prospective, multicenter validation study. Intensive Care Med 39:583–592
Guerin C, Reignier J, Richard JC et al (2013) Prone positioning in severe acute respiratory distress syndrome. N Engl J Med 368:2159–2168
Esteban A, Frutos-Vivar F, Muriel A et al (2013) Evolution of mortality over time in patients receiving mechanical ventilation. Am J Respir Crit Care Med 188:220–230
Demoule A, Jaber S, Kouatchet A et al (2012) Increased use of non-invasive ventilation and changes in indications among French ICUs: the 2011 oVNI study. Am J Respir Crit Care Med 185:A3107
Phillips CR (2013) The Berlin definition: real change or the emperor’s new clothes? Crit Care 17:174
Pintado MC, de Pablo R, Trascasa M et al (2013) Individualized PEEP setting in subjects with ARDS: a randomized controlled pilot study. Respir Care 58:1416–1423
Britos M, Smoot E, Liu KD et al (2011) The value of positive end-expiratory pressure and Fio(2) criteria in the definition of the acute respiratory distress syndrome. Crit Care Med 39:2025–2030
Briel M, Meade M, Mercat A et al (2010) Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA 303:865–873
Mercat A, Richard JC, Vielle B et al (2008) Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA 299:646–655
Meade MO, Cook DJ, Guyatt GH et al (2008) Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA 299:637–645
Rubenfeld GD, Caldwell E, Peabody E et al (2005) Incidence and outcomes of acute lung injury. N Engl J Med 353:1685–1693
Linko R, Okkonen M, Pettila V et al (2009) Acute respiratory failure in intensive care units. FINNALI: a prospective cohort study. Intensive Care Med 35:1352–1361
Sigurdsson MI, Sigvaldason K, Gunnarsson TS, Moller A, Sigurdsson GH (2013) Acute respiratory distress syndrome: nationwide changes in incidence, treatment and mortality over 23 years. Acta Anaesthesiol Scand 57:37–45
Pham T, Combes A, Roze H et al (2013) Extracorporeal membrane oxygenation for pandemic influenza A(H1N1)-induced acute respiratory distress syndrome: a cohort study and propensity-matched analysis. Am J Respir Crit Care Med 187:276–285
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Take-home message: The present study did not validate the Berlin definition of ARDS. Neither the stratification by severity nor the PaO2/FiO2 at study entry was independently associated with mortality.
For the REALYS network, Lyon, France.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hernu, R., Wallet, F., Thiollière, F. et al. An attempt to validate the modification of the American-European consensus definition of acute lung injury/acute respiratory distress syndrome by the Berlin definition in a university hospital. Intensive Care Med 39, 2161–2170 (2013). https://doi.org/10.1007/s00134-013-3122-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-013-3122-6