Abstract
Purpose
To determine incidence, risk factors and outcome of tracheal ischemic lesions related to intubation.
Methods
Planned post hoc analysis using patients from a previous randomized controlled study. Fiberoptic tracheoscopy was performed during the 24 h following extubation. In patients with >2 ischemic lesions, ulcer or tracheal rupture, fiberoptic tracheoscopy was repeated 2 weeks after the last extubation. Tracheal ischemic lesions were predefined based on a quantitative score.
Results
Ninety-six adult patients were included in this study. Eighty (83 %) patients had at least one tracheal ischemic lesion. Thirty-seven (38 %) patients had a tracheal ischemia score > median score (5; IQ 1, 7). The most common tracheal ischemic lesion was ischemia (68 %), followed by hyperemia (54 %), ulcer (10 %), and tracheal rupture (1 %). Univariate analysis identified duration of neuromuscular-blocking agent use, overinflation of tracheal cuff (>30 cmH2O), percentage of P cuff determination >30 cmH2O, duration of assist-control ventilation, and plateau pressure as risk factors for having a tracheal ischemia score >5. Duration of assist-control mechanical ventilation was the only factor independently associated with tracheal ischemia score >5 [OR (95 % CI) 1.10 per hour (1.02–1.20)]. A fiberoptic tracheoscopy was performed 2 weeks after extubation in 22 patients. This examination was normal in all patients, except the one with tracheal rupture who had marked improvement.
Conclusion
Tracheal ischemic lesions are common in intubated, critically ill patients. Duration of assist-control mechanical ventilation through a tracheal tube is the only independent risk factor. These lesions healed in the majority of patients 2 weeks after extubation.
Similar content being viewed by others
Introduction
Tracheal ischemia is a late-onset complication of intubation. Tracheal ischemic lesions are common in critically ill patients intubated with high-volume, low-pressure polyvinyl chloride-cuffed tracheal tubes [1, 2]. Animal and human studies identified overinflation of the tracheal cuff (>30 cmH2O) [3–5], arterial hypotension [6], hypoxemia [2, 7], inflammation [8], and subglottic aspiration [9] as risk factors for tracheal ischemic lesions. Tracheal stenosis, tracheal rupture, tracheobronchial malacia, tracheoinnominate artery fistula, and tracheoesophageal fistula are potential complications of tracheal ischemia [10–16]. These severe complications are associated with important morbidity and mortality.
The severity of tracheal ischemic lesions and subsequent complications have decreased since the replacement of low-volume, high-pressure by high-volume, low-pressure tracheal tubes which allow tracheal sealing with a lower cuff pressure (P cuff) [17, 18]. However, little data are available on this important intubation-related complication. Only two studies performed during the early 80s investigated tracheal ischemic lesions in critically ill patients intubated with high-volume low-pressure tracheal tubes [1, 2]. Based on the results of these studies, tracheal ischemic lesions occur in 31–95 % of patients. However, the limitations of these studies should be taken into account. In the study performed by Kastanos and colleagues [2], only a small number of patients (n = 19) were included. In addition, no quantitative score was defined to evaluate ischemic lesions. Although Stauffer and colleagues [1] included a large number of intubated patients (n = 150), only 41 intubated patients could be evaluated for ischemic tracheal lesions. In addition, no evaluation using fiberoptic tracheoscopy was performed in the study patients, and the only evaluation of tracheal ischemic lesions was performed postmortem. Therefore, we performed this planned post hoc study to determine the incidence, risk factors, and outcome of tracheal ischemic lesions.
Patients and methods
The aim of this planned post hoc analysis was to determine the incidence, risk factors, and outcome of tracheal ischemic lesions in intubated, critically ill patients. Only patients with at least one fiberoptic tracheoscopy were included in this study.
Design of the initial randomized trial
The initial prospective randomized controlled trial was conducted in a single ten-bed medical ICU during an 11-month period (ClinicalTrials.gov NCT01082666) [19]. The study was approved by the institutional review board of the Lille University Hospital. Written consent was obtained from the patients or their proxies. The primary outcome was the impact of continuous control of P cuff on microaspiration of gastric contents. The impact of this intervention on tracheal ischemic lesions was one of the secondary outcomes.
Patients >18 years, intubated and expected to require mechanical ventilation for at least 48 h were eligible for the study. Patients were excluded if they (1) were already enrolled in another trial, (2) had a contraindication for semirecumbent position, (3) had a contraindication for enteral nutrition, (4) had already undergone mechanical ventilation for >48 h at the time of screening for eligibility, (5) were admitted to the ICU with prior tracheostomy.
Patients were randomly assigned to receive continuous control of P cuff (intervention group) or routine care (control group). In both groups, management of the P cuff was continued until the end of mechanical ventilation or death. Target P cuff was 25 cmH2O. In the intervention group, continuous control of cuff pressure was performed using a pneumatic device (Nosten®, Leved, St-Maur, France). In the control group, routine care of tracheal cuff was performed using a manual manometer (Ambu® Cuff Pressure Gauge, Ambu A/S, Ballerup, Denmark) to check and adjust P cuff thrice a day.
Tracheal tube size was 7.5, and 8 in women and men, respectively. All tracheal tubes used in this study were high-volume, low-pressure polyvinyl chloride-cuffed. No subglottic aspiration was performed in study patients. Systemic corticosteroids were not used to prevent post-extubation laryngeal oedema.
Diagnosis of tracheal ischemic lesions
Tracheal ischemic lesions were defined according to a score based on the presence of hyperaemia, ischemia, ulcer, and tracheal rupture. These lesions were defined as moderate, severe, or confluent (Table 1). This score was based on previously described tracheal ischemic lesions and on personal unpublished data. A literature review of clinical and histological studies [1, 2, 20, 21] and our clinical experience suggested that hyperaemia, ischemia, ulcer, and tracheal rupture were the most frequently described intubation-related lesions. In order to take into account the severity of these lesions, they were classified into moderate, severe, and confluent based on the number of lesions. Fiberoptic tracheoscopy was performed by two pneumologists (CF and PhR). CF was always contacted first and performed the majority of tracheoscopies [64 of 96 (66 %)]. In addition, when fiberoptic tracheoscopy was performed by PhR, the examination was recorded and interpreted by CF. The interpretation of CF was only used to classify patients in this study. However, the two interpretations (CF and PhR) were used to calculate inter-observer variability. Pneumologists were blinded to group assignment. In addition, their observations were independent.
Fiberoptic tracheoscopy was performed in all patients during the 24 h following extubation to evaluate tracheal ischemic lesions. In patients with more than one fiberoptic tracheoscopy, because of extubation failure, the tracheal ischemia score obtained during the last tracheoscopy was used. In patients who required percutaneous tracheostomy, fiberoptic tracheoscopy was performed during the procedure. Fiberoptic tracheoscopy could not be performed in patients who died before extubation. No post-mortem evaluation of tracheal ischemia was performed. In patients with >2 ischemic lesions, ulcer, or tracheal rupture; fiberoptic tracheoscopy was planned 2 weeks after the last extubation.
Data collection
All data were prospectively recorded. The following characteristics were recorded at ICU admission: age, gender, severity of illness based on Simplified Acute Physiology Score II, Logistic Organ Dysfunction Score, McCabe Score, comorbidities (diabetes, COPD, chronic heart failure, cirrhosis, chronic renal failure requiring dialysis, immunosuppression), body mass index, hypoalbuminemia (<20 g/l), intubation before ICU admission, and causes for ICU admission. The following data were collected during ICU stay: continuous control of P cuff, vasopressor use, sedation, neuromuscular-blocking agent use, corticosteroids, red blood cell transfusion, size of tracheal tube, self extubation, reintubation, tracheostomy, ventilator-associated tracheobronchitis [22], tracheobronchial colonization [19], P cuff, overinflation (>30 cmH2O) and underinflation (<20 cmH2O) of tracheal cuff, duration of intubation, type and duration of respiratory modes through a tracheal tube, airway pressures, duration of mechanical ventilation, length of ICU stay, ICU-mortality.
Statistical analysis
SPSS software (SPSS, Chicago, IL) was used for data analysis. All p values were two-tailed. Differences were considered significant if p < 0.05. Categorical variables were described as frequencies (%). The distribution of continuous variables was tested for normality. Normally distributed and skewed continuous variables were described as mean ± SD and median [interquartile range (IR)], respectively.
The median tracheal ischemic score was determined in all included patients. Based on this score, patients were classified in two groups: severe tracheal ischemic lesions (tracheal ischemia score > median score), and no severe tracheal ischemic lesions (tracheal ischemia score ≤ median score). In order to determine risk factors for tracheal ischemic lesions, the two groups were compared using univariate and multivariate analyses. Chi-square test or Fischer’s exact test were used to compare qualitative variables, as appropriate. Student’s t-test or Mann–Whitney U test were used to compare normally distributed and skewed continuous variables, as appropriate. All data from univariate analysis with p values <0.1 were incorporated in the multivariate logistic regression analysis. Potential interactions were tested, and the Hosmer–Lemshow goodness-of-fit was calculated. OR (95 % CI) were calculated for all significant qualitative variables in univariate analysis, and all significant variables in multivariate analysis.
In the subgroup of patients (n = 32) in which fiberoptic tracheoscopy was recorded and interpreted by two pneumologists, the inter-rater agreement was assessed using the intra-class correlation coefficient according to the Fleiss method.
Results
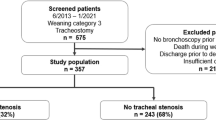
Ninety-six patients were included in this study. All of these patients had at least one fiberoptic tracheoscopy during the 24 h following extubation. These patients represented 78 % of the 122 patients included in the initial randomized controlled trial, and 74 % of the 129 patients eligible for that trial. Twenty-six of 122 (21 %) patients were not included in this study because tracheoscopy could not be performed since they died before extubation. Interobserver coefficient of reproducibility was 0.953.
Thirty-seven patients (38 %) had a tracheal ischemia score > median score (5; interquartile range 1, 7). The distribution of tracheal ischemia score is presented in Fig. 1. Fiberoptic tracheoscopy was well tolerated in all patients and no complication was reported. Eighty patients (83 %) had at least one tracheal ischemic lesion. The most frequent lesion was ischemia [66 patients (68 %)], followed by hyperemia [52 patients (54 %)], ulcer [10 patients (10 %)] (Fig. 2), and tracheal rupture [1 patient (1 %)] (Table 2). All these lesions were located at the cuff contact area. No granuloma or stenosis were diagnosed in study patients. The patient with tracheal rupture had no clinical or radiologic signs of tracheal rupture. This patient was intubated at the emergency department 10 h before ICU admission. A P cuff of 90 cmH2O was measured at ICU admission. No difficult intubation was reported by the emergency department physician who declared that P cuff was not routinely measured in their department. Median duration of mechanical ventilation in study patients was 8 days (Interquartile range 5, 15 days). No significant difference was found in tracheal ischemia score or type of these lesions between patients with duration of mechanical ventilation >8 days and those with duration of mechanical ventilation ≤8 days, or between patients with or without continuous control of P cuff (Table 2). We found that P cuff was significantly higher in patients receiving continuous control of P cuff compared with those receiving routine care of tracheal cuff [median (IR) 25 (24, 26) vs 22 (21, 24) cmH2O, respectively; p < 0.001). Tracheal ischemia score and percentage of patients with tracheal ischemia score > median were similar in patients with continuous control of P cuff compared with those with routine care and P cuff > 30 cmH2O, or those with routine care and P cuff ≤ 30 cmH2O, and in patients with routine care and P cuff > 30 cmH2O compared with those with routine care and P cuff ≤ 30 cmH2O (p > 0.2 for all comparisons).
No significant difference was found in patient characteristics at ICU admission (Table 3). Univariate analysis identified duration of neuromuscular-blocking agent use, overinflation of tracheal cuff, % of P cuff determinations >30, duration of assist-control ventilation, plateau pressure as risk factors for tracheal ischemia score >5. Other patient characteristics were similar during ICU stay (Table 4). Moderate laryngeal dyspnea occurred in two patients. No significant relationship (p > 0.9) was found between laryngeal dyspnea and tracheal ischemia score. Multivariate analysis identified duration of assist-control ventilation as the only independent risk factor for tracheal ischemia score >5 [OR (95 % CI) 1.10 per hour (1.02–1.20), p = 0.015] (Lemshow goodness-of-fit test, p = 0.296). No significant difference was found in duration of mechanical ventilation (median 10 days (5, 21) vs 7 days (5, 15), p = 0.234), length of ICU stay (median 13 days (IQ 7, 22) vs 11 (7, 18), p = 0.512], and mortality [7 of 37 (18 %) vs 8 of 59 (13 %), p = 0.618] between patients with tracheal ischemia score >5 and those with tracheal ischemia score ≤5, respectively.
Among the 35 (36 %) patients in whom severity of tracheal ischemic lesions justified a fiberoptic tracheoscopy 2 weeks after extubation, 22 (62 %) patients underwent a fiberoptic tracheoscopy. Fiberoptic tracheoscopy could not be performed in 13 patients because six patients died before ICU discharge, four patients were tracheostomized, and three patients refused this examination. Fiberoptic tracheoscopy, performed 2 weeks after extubation, was well tolerated in all patients and no complication was reported. In all patients, except the one with tracheal rupture, no tracheal ischemic lesion was found at 2 weeks after extubation. In the patient with tracheal rupture, a marked improvement was found and the patient refused subsequent fiberoptic tracheoscopy. However, no subsequent clinical complications related to tracheal rupture occurred in this patient.
Discussion
Our results suggest that tracheal ischemic lesions are common in intubated, critically ill patients. Duration of assist-control ventilation through a tracheal tube was the only independent risk factor for severe tracheal ischemic lesions. A favourable outcome of tracheal ischemic lesions was found in the majority of patients with severe lesions. These results suggest the lack of clinically significant ischemic complications related to the tracheal cuff, at least when P cuff is maintained in a safe range.
The incidence of tracheal ischemic lesions found by our study (83 %) is higher than that reported by Kastanos and colleagues [2] (31 %). However, in their study, fiberoptic tracheoscopy was performed during the 2 weeks following extubation (often 10 days after extubation), suggesting that the incidence was probably underestimated. Stauffer and colleagues [1] reported higher incidence of tracheal ischemic lesions (95 %). However, this was a post-mortem study, and no information on survivors could be provided. Our study is the first reporting on tracheal ischemic lesions in a large cohort of patients using an early (24 h after extubation) tracheoscopy.
Duration of assist-control ventilation through a tracheal tube was the only independent risk factor for tracheal ischemic lesions. This might be explained by the fact that P cuff is correlated to airway pressure which is higher during assist-control ventilation compared with pressure support and bilevel positive pressure ventilation. This result suggests that pressure support ventilation should be preferred in critically ill patients in order to prevent tracheal ischemic lesions. However, further studies are needed to confirm this result. Previous clinical studies identified P cuff, female gender, older age, duration of intubation, hypoxemia, and positive end-expiratory pressure as risk factors for tracheal ischemic lesions by univariate analysis [1–3]. However, none of these studies has adjusted for potential confounders by multivariate analysis.
No significant difference was found in tracheal ischemic lesions between patients with continuous control of P cuff and those with routine care of the tracheal cuff. Several potential explanations could be provided for this result. The impact of continuous control of P cuff on tracheal ischemic lesions was a secondary objective. Therefore, the study is probably underpowered to detect a significant difference in this outcome. Another possible explanation is the fact that routine care of the tracheal cuff was probably optimal in the control group. A recent randomized controlled study performed in a large number of patients scheduled for elective surgery found that proper control of P cuff using a manometer was associated with significantly reduced clinical signs related to cuff overinflation compared with no measurement of P cuff [23]. Further, previous studies showed that overinflation of the tracheal cuff was not permanent, and occurred during coughing, patient mobilization and patient–ventilator asynchrony [21, 24–26]. A previous study showed that overinflation of the tracheal cuff for up to 30 min was associated with significantly reduced but completely reversible ischemia [3]. Therefore, short overinflation of tracheal cuff might not be harmful in critically ill patients, and continuous control of P cuff would not add much in this scenario. Finally, another explanation could be the higher P cuff in patients receiving continuous control of P cuff compared with those receiving routine care, even if the median P cuff is <30 cmH2O. A randomized controlled animal study found tracheal ischemic lesions in animals intubated and ventilated for 48 h despite continuous control of P cuff (<30 cmH2O) [21]. Further randomized controlled studies are needed to determine the impact of continuous control of P cuff on tracheal ischemic lesions.
Our results suggest the absence of significant morbidity related to tracheal ischemic lesions. However, fiberoptic tracheoscopy was performed 2 weeks after extubation in a small number of patients (n = 22). This result should be confirmed by further large multicenter studies.
Some limitations of our study should be taken into account. The study was performed in a single medical ICU. Therefore, our results could not be extrapolated to patients in other ICUs. In addition, the study was a planned post hoc analysis. However, all data were prospectively collected, and these results could be helpful for future randomized controlled studies on the prevention of tracheal ischemic lesions. Further, because of technical problems, fiberoptic tracheoscopy was interpreted by two physicians in only 33 % of study patients. Another potential limitation is the use of median tracheal ischemia score to classify study patients. The clinical significance of such a classification is unknown. We repeated the risk factor analysis using two other classifications based on 25th and 75th interquartiles. No independent risk factor could be identified for tracheal ischemic lesions using these classifications (results not shown). However, the use of these classifications resulted in small number of patients in some groups, which precludes definite conclusions. Additionally, the number of tracheal suctioning performed during the tracheoscopy could not be provided. It has been reported that few tracheal suctionings could immediately lead to hyperemia. However, hyperaemia was located at the cuff contact area. In addition, tracheal suctioning was not routinely performed during tracheoscopy. Finally, no information could be provided on aspiration, traumatic intubation before ICU admission, or the time of occurrence of tracheal ischemic lesions during mechanical ventilation.
We conclude that tracheal ischemic lesions are common in intubated critically ill patients. The duration of assist-control ventilation is the only independent risk factor for these lesions. The majority of severe tracheal ischemic lesions resolved 2 weeks after extubation. Our results suggest that fiberoptic tracheoscopy could not be recommended in asymptomatic, critically ill patients after extubation, provided that appropriate routine care of tracheal cuff was performed during intubation and mechanical ventilation.
Abbreviations
- ICU:
-
Intensive care unit
- IR:
-
Interquartile range
- P cuff :
-
Cuff pressure
References
Stauffer JL, Olson DE, Petty TL (1981) Complications and consequences of endotracheal intubation and tracheotomy. A prospective study of 150 critically ill adult patients. Am J Med 70:65–76
Kastanos N, Estopá Miró R, Marín Perez A, Xaubet Mir A, Agustí-Vidal A (1983) Laryngotracheal injury due to endotracheal intubation: incidence, evolution, and predisposing factors. A prospective long-term study. Crit Care Med 11:362–367
Seegobin RD, van Hasselt GL (1981) Endotracheal cuff pressure and tracheal mucosal blood flow: endoscopic study of effects of four large volume cuffs. Br Med J 288:965–968
Nordin U (1977) The trachea and cuff-induced tracheal injury. An experimental study on causative factors and prevention. Acta Otolaryngol Suppl 345:1–71
Touzot-Jourde G, Stedman NL, Trim CM (2005) The effects of two endotracheal tube cuff inflation pressures on liquid aspiration and tracheal wall damage in horses. Vet Anaesth Analg 32:23–29
Bunegin L, Albin MS, Smith RB (1993) Canine tracheal blood flow after endotracheal tube cuff inflation during normotension and hypotension. Anesth Analg 76:1083–1090
Gordin A, Chadha NK, Campisi P, Luginbuehl I, Taylor G, Forte V (2011) An animal model for endotracheal tube-related laryngeal injury using hypoxic ventilation. Otolaryngol Head Neck Surg 144:247–251
Puyo CA, Tricomi SM, Dahms TE (2008) Early biochemical markers of inflammation in a swine model of endotracheal intubation. Anesthesiology 109:88–94
Berra L, De Marchi L, Panigada M, Yu ZX, Baccarelli A, Kolobow T (2004) Evaluation of continuous aspiration of subglottic secretion in an in vivo study. Crit Care Med 32:2071–2078
Conti M, Pougeoise M, Wurtz A, Porte H, Fourrier F, Ramon P, Marquette CH (2006) Management of postintubation tracheobronchial ruptures. Chest 130:412–418
Brichet A, Verkindre C, Dupont J, Carlier ML, Darras J, Wurtz A, Ramon P, Marquette CH (1999) Multidisciplinary approach to management of postintubation tracheal stenoses. Eur Respir J 13:888–893
Makris D, Dimoulis A, Marquette CH, Zakynthinos E (2010) A 73-year-old woman with tracheobronchiomalacia. Intensive Care Med 36:1441–1442
Hameed AA, Mohamed H, Al-Mansoori M (2008) Acquired tracheoesophageal fistula due to high intracuff pressure. Ann Thorac Med 3:23–25
Marty-Ané CH, Picard E, Jonquet O, Mary H (1995) Membranous tracheal rupture after endotracheal intubation. Ann Thorac Surg 60:1367–1371
Sessa C, Costache V, Porcu P, Thony F, Blin D, Brichon PY, Magne JL (2006) Tracheoinnominate artery fistula: combined endovascular and surgical management by emergency stent-graft placement followed by cryopreserved arterial allograft repair. Ann Vasc Surg 20:731–735
Spittle N, McCluskey A (2000) Lesson of the week: tracheal stenosis after intubation. BMJ 321:1000–1002
Honeybourne D, Costello JC, Barham C (1982) Tracheal damage after endotracheal intubation: comparison of two types of endotracheal tubes. Thorax 37:500–502
Loeser EA, Hodges M, Gliedman J, Stanley TH, Johansen RK, Yonetani D (1978) Tracheal pathology following short-term intubation with low- and high-pressure endotracheal tube cuffs. Anesth Analg 57:577–579
Nseir S, Zerimech F, Fournier C, Lubret R, Ramon P, Durocher A, Balduyck M (2011) Continuous control of tracheal cuff pressure and microaspiration of gastric contents in critically ill patients. Am J Respir Crit Care Med 184:1041–1047
Combes X, Schauvliege F, Peyrouset O, Motamed C, Kirov K, Dhonneur G, Duvaldestin P (2001) Intracuff pressure and tracheal morbidity: influence of filling with saline during nitrous oxide anesthesia. Anesthesiology 95:1120–1124
Nseir S, Duguet A, Copin MC, De Jonckheere J, Zhang M, Similowski T, Marquette CH (2007) Continuous control of endotracheal cuff pressure and tracheal wall damage: a randomized controlled animal study. Crit Care 11:R109
Nseir S, Di Pompeo C, Pronnier P, Beague S, Onimus T, Saulnier F, Grandbastien B, Mathieu D, Delvallez-Roussel M, Durocher A (2002) Nosocomial tracheobronchitis in mechanically ventilated patients: incidence, aetiology and outcome. Eur Respir J 20:1483–1489
Liu J, Zhang X, Gong W, Li S, Wang F, Fu S, Zhang M, Hang Y (2010) Correlations between controlled endotracheal tube cuff pressure and postprocedural complications: a multicenter study. Anesth Analg 111:1133–1137
Duguet A, D’Amico L, Biondi G, Prodanovic H, Gonzalez-Bermejo J, Similowski T (2007) Control of tracheal cuff pressure: a pilot study using a pneumatic device. Intensive Care Med 33:128–132
Sole ML, Su X, Talbert S, Penoyer DA, Kalita S, Jimenez E, Ludy JE, Bennett M (2011) Evaluation of an intervention to maintain endotracheal tube cuff pressure within therapeutic range. Am J Crit Care 20:109–117
Servin SO, Barreto G, Martins LC, Moreira MM, Meirelles L, Neto JA, Zen Júnior JH, Tincani AJ (2011) Atraumatic endotracheal tube for mechanical ventilation. Rev Bras Anestesiol 61:311–319
Conflicts of interest
SN has participated in an advisory board organised by Covidien, other authors: None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Touat, L., Fournier, C., Ramon, P. et al. Intubation-related tracheal ischemic lesions: incidence, risk factors, and outcome. Intensive Care Med 39, 575–582 (2013). https://doi.org/10.1007/s00134-012-2750-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-012-2750-6