Abstract
Objective
Noninvasive ventilation (NIV) is often applied with ICU ventilators. However, leaks at the patient-ventilator interface interfere with several key ventilator functions. Many ICU ventilators feature an NIV-specific mode dedicated to preventing these problems. The present bench model study aimed to evaluate the performance of these modes.
Design and setting
Bench model study in an intensive care research laboratory of a university hospital.
Methods
Eight ICU ventilators, widely available in Europe and featuring an NIV mode, were connected by an NIV mask to a lung model featuring a plastic head to mimic NIV conditions, driven by an ICU ventilator imitating patient effort. Tests were conducted in the absence and presence of leaks, the latter condition with and without activation of the NIV mode. Trigger delay, trigger-associated inspiratory workload, and pressurization were tested in conditions of normal respiratory mechanics, and cycling was also assessed in obstructive and restrictive conditions.
Results
On most ventilators leaks led to an increase in trigger delay and workload, a decrease in pressurization, and delayed cycling. On most ventilators the NIV mode partly or totally corrected these problems, but with large variations between machines. Furthermore, on some ventilators the NIV mode worsened the leak-induced dysfunction.
Conclusions
The results of this bench-model NIV study confirm that leaks interfere with several key functions of ICU ventilators. Overall, NIV modes can correct part or all of this interference, but with wide variations between machines in terms of efficiency. Clinicians should be aware of these differences when applying NIV with an ICU ventilator.
Similar content being viewed by others
Introduction
Noninvasive ventilation (NIV) in pressure support mode (PS) has become a standard of care in the management of patients with acute respiratory failure [1–3]. Patient tolerance to NIV is a key element to its success in avoiding intubation [4, 5]. One of the most important factors known to decrease tolerance to NIV is the presence of major leaks at the patient-mask interface, as leaks can interfere with several key aspects of ventilator function [6–9], thereby leading to patient-ventilator asynchrony [10, 11] and increasing the risk of failure of NIV [5, 12]. The tight fitting of a properly selected NIV mask reduces the magnitude of leaks, but this measure alone often proves insufficient [12] and can be limited by skin complications and patient discomfort [13]. Therefore enhancing ventilator performance to minimize the negative impact of leaks is an important avenue of development. Most devices used for long-term home ventilation have been designed to deal with leaks and are often capable of adequate triggering [14] and ventilation despite their presence [15], albeit with large variations between machines [16]. ICU ventilators, on the other hand, were originally designed to ventilate intubated patients, i. e., with minimal or no leaks, and fare less well in their presence [14]. However, given that these machines have been increasingly used for NIV over the years, manufacturers have developed “NIV modes” which aim to minimize the impact of leaks on key ventilator functions.
The purpose of this study was to test the performance of NIV modes of several recent ICU ventilators in PS in the absence and presence of leaks on a specially designed NIV bench model. Findings of this study were presented in abstract form at the 2006 Annual Congress of the European Society of Intensive Care Medicine.
Methods
Ventilators
All current ICU ventilators commonly distributed in Europe in which a specific NIV mode is presently implemented were tested: Elysée (ResMed-Saime, North Ryde, Australia), Esprit (Respironics, Murryville Pa., USA), Evita XL (Drägerwerk, Lübeck, Germany), Extend (Taëma, Anthony, France), Newport e500 (Newport Medical Instruments, Costa Mesa Calif., USA), Servo i (Maquet, Solna, Sweeden), Vela (Viasys Healthcare, Palm Springs Calif., USA), and Raphael (Hamilton Medical, Rhäzuns, Switzerland). Three ventilators (Galileo, Hamilton Medical, Rhäzuns, Switzerland; Avea, Viasys Healthcare; Engström Carestation, GE Healthcare, Fairfield, Conn., USA) which at the time of the tests were equipped with only a compensation of leaks at the endotracheal tube cuff were excluded from the study as this does not represent a true NIV mode designed to cope with much larger leaks. Details of each ventilator's NIV mode are summarized in the Electronic Supplementary Material (ESM).
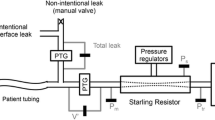
NIV bench model
The model is described in detail in the ESM. It was derived from that used in previous studies from our group [17, 18], adapted to model NIV conditions with and without leaks. Briefly, the model consists of two separate chambers linked by a rigid metal strip. One chamber mimics patient inspiratory effort, which is detected as an “inspiratory” effort by the tested ventilator, which in turn triggers a pressure support response. To model NIV conditions a PVC head (Bill I, VBM Medizintechnik, Sulz, Germany) equipped with upper airways and a trachea was used, connected to the tested ventilator by an adult medium size oronasal NIV mask. A three-way stopcock was inserted in the circuit between the Y-piece and the mask to generate a leak. All measurements were performed at an FIO2 of 0.21. Data were acquired online and stored in a laptop computer for subsequent analysis (Acqknowledge software, Biopac Systems, Goleta, Calif., USA).
Measured parameters
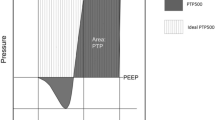
The tracing analysis allowed determination of several key parameters of pressure supported breaths, namely (see ESM for detailed explanation): triggering: triggering delay (Td), trigger pressure drop (ΔPtrigger), inspiratory pressure-time product (PTPt), and autotriggering; pressurization: pressure-time products at 300 and 500 ms for each respiratory cycle (PTP300 and PTP500); inspiratory:expiratory cycling: the duration of pressurization by the ventilator in excess (positive value, delayed cycling) or in deficit (negative value, premature cycling) of the patient inspiratory time (tipat) was determined.
Leaks
The mean leak volume per minute was determined by comparing mask and tracheal flow curves (see ESM).
Experimental protocol
The driving ventilator was set in airway pressure release ventilation mode. Triggering and pressurization were tested with normal respiratory mechanics and cycling in normal, obstructive and restrictive conditions. The ventilators were tested in PS mode, with PS level 15 cmH2O; PEEP 5 cmH2O; inspiratory flow trigger; pressurization slope at its steepest value without premature cycling; cycling 25% of peak inspiratory flow; if adjustable, the inspiratory time was set to its maximum. The tests were performed in three conditions: (a) PS mode and no leak (L0/NIV0), (b) PS and leak (L+/NIV0), and (c) PS plus NIV-specific mode and leak (L+/NIV+). Each condition was tested for 15 min.
Statistical analysis
All results are expressed as mean ± SD. For all conditions ten measurements were obtained and averaged. The results of the different conditions were compared by analysis of variance on ranks. Δti with and without leaks, and with and without NIV specific mode were compared by analysis of variance. A p value less than 0.05 was considered statistically significant.
Results
Leak
In baseline conditions a minimal leak volume averaging 2.2 ± 0.7 l/min was present despite adequate mask fitting and strap tightening, which had no impact on ventilator function. The mean leak volume during the triggering and pressurization experiments leak conditions (L+/NIV0 and L+/NIV+) were: 12.9 ± 2.2 l/min for L+/NIV0 and 13.1 ± 1.9 l/min for L+/NIV+. In the various respiratory mechanics conditions used for cycling evaluation the mean leak volume was 12.6 ± 1.8 (normal), 13.2 ± 2.3 (obstructive), and 12.8 ± 1.9 l/min (restrictive), respectively (difference NS). The mean leak volume was close to the mean minute-volume, i. e., on average leaks represented approx. 100% of tidal volume. The leak was partitioned between the obligatory leak around the mask (17%) and the leak through the calibrated orifice (83%).
Autotriggering
No autotriggering occurred in the absence of leaks, while all machines except the Vela autotriggered with leaks. On the Evita XL it proved impossible to avoid severe autotriggering with leaks, which persisted despite maximal reduction in trigger sensitivity. Consequently no valid measurements could be made in the L+/NIV0 mode with this machine, as described with other ventilators presenting this same problem [14]. Autotriggering was completely corrected by NIV modes in all ventilators.
Inspiratory trigger
In the absence of leaks all machines except two (Elysée and Newport) had a Td of 100 ms or less (Fig. 1). With leaks Td increased in four ventilators (Elysée, Extend, Raphael, Vela), remained unchanged in two (Esprit and Servo i), and decreased in one (Newport e500). Td was not measurable with the Evita XL due to persistent autotriggering. With leaks and NIV mode activated, Td decreased in three of the four ventilators in which it was increased by leaks (Elysée, Extend, Vela), and remained unchanged in the Raphael. In the two machines initially unaffected by leaks, NIV mode led to an absence of change in the Esprit, and to a marked increase in the Servo i. Finally, NIV mode increased Td in the Newport e500. On the Evita XL NIV mode decreased Td compared to baseline conditions, no comparison being possible with the leak/no NIV mode condition.
Trigger delay (Td) with the eight ICU ventilators tested with normal respiratory mechanics under three conditions: no leaks and no NIV mode (L0.NIV0), leaks and no NIV mode (L+.NIV0), leaks and NIV mode (L+.NIV+). Td was not measurable with the Evita XL due to severe autotriggering despite trigger threshold adjustments. Histogram bars Mean ± SD. § p < 0.05 vs. L0.NIV0, ♣ p < 0.05 vs. L+.NIV0 (analysis of variance), ∗impossible to measure because of autotriggering
With the exception of the Newport e500, in the absence of leaks all machines had values of ΔP and PTPt lower than 1 cmH2O and 0.06 cmH2O/s, respectively (Figs. 2, 3). Leaks increased ΔP and PTPt in all machines except the Esprit (unchanged) and the Newport e500 (decreased). ΔP and PTPt were reduced by the NIV mode in three machines (Esprit, Extend, and Raphael) and increased in four (Elysée, Newport e500, Servo i, Vela). On the Evita XL NIV mode decreased ΔP and PTPt compared to baseline conditions, no comparison being possible with the leak/no NIV mode condition.
Inspiratory trigger pressure drop (ΔP trigger) with the eight ICU ventilators tested with normal respiratory mechanics under three conditions: no leaks and no NIV mode (L0.NIV0), leaks and no NIV mode (L+.NIV0), leaks and NIV mode (L+.NIV+). Histogram bars Mean ± SD. § p < 0.05 vs. L0.NIV0, ♣ p < 0.05 vs. L+.NIV0 (analysis of variance), ∗impossible to measure because of autotriggering
Inspiratory trigger pressure-time product (PTP t ) with the eight ICU ventilators tested with normal respiratory mechanics under three conditions: no leaks and no NIV mode (L0.NIV0), leaks and no NIV mode (L+.NIV0), leaks and NIV mode (L+.NIV+). Histogram bars Mean ± SD. § p < 0.05 vs. L0.NIV0, ♣ p < 0.05 vs. L+.NIV0 (analysis of variance), ∗impossible to measure because of autotriggering
Pressurization
Results being comparable, only the PTP500 is reported. In five ventilators leaks reduced PTP500, the magnitude of the decrease varying between machines (Elysée, Esprit, Extend, Raphael, Vela; Fig. 4). In two of these devices PTP500 was partly (Extend) or more than completely (Raphael) corrected by the NIV mode while it was unchanged in two others (Elysée, Esprit) and decreased further in one (Vela). PTP500 was unaffected by leaks in the Servo i, but was reduced by the NIV mode. In the Newport PTP500 was increased with leaks, and the increase was attenuated by the NIV mode. Finally on the Evita XL PTP500 was lower with the NIV mode than in baseline conditions, but no comparison could be made in conditions of leak/no NIV mode.
Pressure time product at 500 ms (PTP 500) with the eight ICU ventilators tested under three conditions: no leaks and no NIV mode (L0.NIV0), leaks and no NIV mode (L+.NIV0), leaks and NIV mode (L+.NIV+). Histogram bars Mean ± SD. § p < 0.05 vs. L0.NIV0, ♣ p < 0.05 vs. L+.NIV0 (analysis of variance), ∗impossible to measure because of autotriggering
PEEP
In all but two ventilators (Esprit, Raphael) leaks led to a moderate (Servo i, Vela) or severe (Elysée, Extend, Newport e500) decrease in the PEEP level (Fig. 5). Overall the NIV mode compensated for leaks on all machines, PEEP always being above 4 cmH2O (set PEEP 5 cmH2O).
Minimum PEEP maintained with the eight ICU ventilators tested with normal respiratory mechanics under three conditions: no leaks and no NIV mode (L0.NIV0), leaks and no NIV mode (L+.NIV0), leaks and NIV mode (L+.NIV+). Histogram bars Mean ± SD. § p < 0.05 vs. L0.NIV0, ♣ p < 0.05 vs. L+.NIV0 (analysis of variance), ∗impossible to measure because of autotriggering
Inspiratory:expiratory cycling
With normal respiratory mechanics (Table 1) and no leaks Δti was between 10% and 20% on seven ventilators, and at 40% on the Elysée. Leaks markedly increased Δti on all machines, a problem which was corrected by NIV mode in three ventilators (Esprit, Evita XL, Servo i), partially addressed in two (Extend, Raphael), unchanged in one (Newport e500), and worsened in two (Elysée, Vela). In obstructive conditions (Table 2) baseline Δti was increased compared to normal mechanics, as expected, which was markedly worsened by leaks, the magnitude of increase in Δti ranging from 100% to 200%, except on the Evita XL (60%). In five ventilators correction by the NIV mode was either complete (Servo i, Esprit, Evita XL the latter two exhibiting a lower Δti than at baseline) or partial (Elysée, Raphael); in three machines no improvement was noted (Newport e500, Extend, Vela the latter two exhibiting a markedly higher Δti). With restrictive mechanics (Table 2) all machines exhibited premature cycling, the magnitude of which was somewhat attenuated by leaks, except for the Extend in which delayed cycling occurred. Compared to baseline, the NIV mode corrected premature cycling in four ventilators (Extend, Newport e500, Raphael, Vela), and worsened it in four others (Elysée, Raphael, Servo i, Evita XL).
Discussion
The results of the present bench model study mimicking NIV conditions confirm that leaks entail major alterations in the key functions of ICU ventilators. They also underline that NIV modes exhibit substantial variability in their ability to cope with these problems. Various limitations of this study should be outlined. First, the model attempts to mimic NIV conditions, but various aspects of patient-ventilator interface (e.g., facial features, mask fit, upper airway muscle activity) are not fully accounted for. Second, the leak was created through a single fixed-diameter orifice, and although its magnitude varied with the pressurization capacity of the tested ventilator, during actual NIV leaks are multifocal and are far more variable than in the model. Another issue is that the level of leak in our model was approx. 100% of true delivered tidal volume, higher than in other bench model studies in which it ranged from 25% to 60% [14, 16, 17] the discrepancy probably stemming from differences in model designs, experimental conditions, and type of ventilators tested. Third, leaks are likely to interfere with triggering parameters such as PTPt. However, leaks were fairly constant throughout the trial. Furthermore, even though leaks can interfere with comparisons between the leak-free baseline and the two other conditions, comparisons between these two conditions should remain valid, provided leaks remain stable, which was the case. Finally, the ventilators were selected on the basis of their being equipped with a true NIV mode, i. e., more than just the ability to compensate for minor leaks around an endotracheal tube cuff. However, this reflects the state of technology when the study was performed, and some machines may have evolved after study completion. These limitations notwithstanding, this type of bench model has been used in several studies [9, 17–19].
Triggering
Without leaks most machines exhibited a very short Td, which is in line with other results found in this generation of ICU ventilators [19]. Predictably leaks increased Td, ΔP and PTPt on all machines except two, albeit with substantial variations between machines. In addition to the effects of the leak itself, these variations likely stem in part from the fact that, to minimize autotriggering we had to raise the flow trigger threshold or resort to pressure triggering [20]. The latter was used in four machines (Elysée, Extend, Newport e500, and Servo i). No increase in Td should have stemmed from the presence of dynamic hyperinflation, given that its absence was verified for each cycle used in the measurements. Moreover, part of the patient effort might become undetectable due to the leaks. The Esprit was unaffected by leaks, which probably results from its technology, directly inspired from single-limb ventilators designed to deal with leaks [14]. No explanation could be found as to why the Newport e500, which at baseline had the highest Td, decreased this delay in the presence of leaks. With NIV mode activated, results varied: Td decreased in three machines (Elysée, Extend, and Vela) increased in two (Newport e500 and Servo i) and was unchanged in two (Esprit and Raphael), while PTPt increased in four machines, two of which had their Td lowered by the NIV mode (Elysée and Vela). This suggests that the satisfactory correction of Td by the NIV mode sometimes comes at the price of a higher workload on, probably because of a slower rate of pressurization. Autotriggering is a major issue with ICU ventilators when faced with leaks, as has been described in other comparable studies [6, 14, 16]. In the study by Miyoshi et al. [14] in particular, home-ventilation devices were little affected by leaks, whereas ICU ventilators exhibited severe autotriggering precluding any valid measurements, as did was the case in our study. NIV mode dealt with this problem efficiently, although this might have also contributed to the rise in Td and PTPt.
Pressurization
Pressurization on most ventilators was markedly decreased by leaks, and benefits little from the NIV mode, only two machines exhibiting an improvement. Mehta et al. [16] also found in a comparable bench study that the pressurization capacity to compensate for leaks varied widely among ventilators. It should be noted that if the NIV mode entails a major increase in Td, such as in the Servo i, this would negatively affect PTP500 (Fig. 4). Therefore the low PTP500 value for this machine with NIV mode probably reflects the increased Td rather than low pressurization ability. Of note, the same holds true for the lower PTP500 found with leaks, i. e., this lower value reflects a combination of increased Td and loss of pressure through leaks. However, the important point from a clinical standpoint is what the patient receives in terms of pressurization, and therefore it is probably not very important to distinguish quantitatively between the two parameters. Again, the Esprit was little affected by leaks, most likely due to its turbine core design specifically tailored to leak conditions. In all ventilators PEEP was maintained with the NIV mode. In our view, this is a major improvement, both for hypoxemic and chronic obstructive pulmonary disease patients, in whom external PEEP can efficiently offset the inspiratory threshold stemming from intrinsic PEEP [21].
Cycling
Without leaks, all ventilators presented some degree of delayed cycling, worsened by obstructive conditions, while restrictive mechanics led to premature cycling. These results are in line with clinical studies [22]. Overall, leaks increased delayed cycling in normal and obstructive conditions, and partly corrected premature cycling with restrictive mechanics. The NIV mode corrected delayed cycling in normal and obstructive mechanics in some machines, but had no effect or worsened the problem in others, the same general observation being made in restrictive conditions. Therefore there was a fairly uneven amount of correction of the effects of leaks on cycling. The clinical relevance of this finding remains to be determined, but cycling is being increasingly recognized as an important component of patient-ventilator interaction [7, 22, 23], and from a theoretical standpoint at least those machines that adequately correct the problem would seem more attractive to provide NIV in certain patients, in particular in those with obstructive mechanics [22, 23].
As a final note, one point which is often raised concerns the safety of using NIV modes in intubated patients. Basically NIV modes aim to compensate for a high level of leaks with the goal of maintaining inspiratory pressure/minute volume and to reset alarm limits accordingly. During the start-up procedure of an ICU ventilator the machine performs a series of autotests of circuit characteristics (compliance and resistance) to compute correction factors for the flow and pressure sensors. Changing to NIV mode once these autotests have been validated could affect ventilator function. Also, many machines in NIV mode compensate for leak flows of up to 30 l/min and do not alarm the clinician before reaching that critical level. Using NIV mode in an intubated patient, in whom there should be no or minimal leaks could carry the risk of not drawing the clinician's attention to the presence of a very large and potentially dangerous leak. Therefore it would seem logical to not use NIV modes in intubated patients.
Conclusion
The results of this bench-model study designed to mimic NIV conditions confirm that leaks interfere with several key functions of ICU ventilators. Overall, NIV modes can correct part or all of this interference, but there are large variations between machines in the efficiency with which their NIV modes handle the various dysfunctions entailed by leaks. The limitations inherent to a bench model study preclude any definite conclusion as to how much these results can be extrapolated to the clinical setting, but such technical information should be kept in mind by clinicians when considering equipment options to perform NIV.
References
Peter JV, Moran JL, Hughes JP (2002) Noninvasive mechanical ventilation in acute respiratory failure—a meta-analysis update. Crit Care Med 30:555–562
Liesching T, Kwok H, Hill NS (2003) Acute applications of noninvasive positive pressure ventilation. Chest 124:699–713
Ferrer M, Esquinas A, Leon M, Gonzalez G, Alarcon A, Torres A (2003) Noninvasive ventilation in severe hypoxemic respiratory failure. Am J Respir Crit Care Med 168:1438–1444
Antonelli M, Conti G, Moro ML, Esquinas A, Gonzalez-Diaz G, Confalonieri M, Pelaia P, Principi T, Gregoretti C, Beltrame F, Pennisi MA, Arcangeli A, Proietti R, Passariello M, Meduri GU (2001) Predictors of failure of noninvasive positive pressure ventilation in patients with acute hypoxemic respiratory failure: a multi-center study. Intensive Care Med 27:1718–1728
Carlucci A, Richard JC, Wysocki M, Lepage E, Brochard L (2001) Noninvasive versus conventional mechanical ventilation. An epidemiologic survey. Am J Respir Crit Care Med 163:874–880
Bernstein G, Knodel E, Heldt GP (1995) Airway leak size in neonates and autocycling of three flow-triggered ventilators. Crit Care Med 23:1739–1744
Calderini E, Confalonieri M, Puccio PG, Francavilla N, Stella L, Gregoretti C (1999) Patient-ventilator asynchrony during noninvasive ventilation: the role of expiratory trigger. Intensive Care Med 25:662–667
Prinianakis G, Delmastro M, Carlucci A, Ceriana P, Nava S (2004) Effect of varying the pressurisation rate during noninvasive pressure support ventilation. Eur Respir J 23:314–320
Schettino GP, Tucci MR, Sousa R, Valente Barbas CS, Passos Amato MB, Carvalho CR (2001) Mask mechanics and leak dynamics during noninvasive pressure support ventilation: a bench study. Intensive Care Med 27:1887–1891
Tobin MJ, Jubran A, Laghi F (2001) Patient-ventilator interaction. Am J Respir Crit Care Med 163:1059–1063
Kondili E, Prinianakis G, Georgopoulos D (2003) Patient-ventilator interaction. Br J Anaesth 91:106–119
Moore MJ, Schmidt GA (2000) Non-invasive ventilation: why does it fail? In Vincent JL (ed) Yearbook of intensive care and emergency medicine. Springer, Berlin Heidelberg New York, pp 318–327
Peerless JR, Davies A, Klein D, Yu D (1999) Skin complications in the intensive care unit. Clin Chest Med 20:453–467
Miyoshi E, Fujino Y, Uchiyama A, Mashimo T, Nishimura M (2005) Effects of gas leak on triggering function, humidification, and inspiratory oxygen fraction during noninvasive positive airway pressure ventilation. Chest 128:3691–3698
Meyer TJ, Pressman MR, Benditt J, McCool FD, Millman RP, Natarajan R, Hill NS (1997) Air leaking through the mouth during nocturnal nasal ventilation: effect on sleep quality. Sleep 20:561–569
Mehta S, McCool FD, Hill NS (2001) Leak compensation in positive pressure ventilators: a lung model study. Eur Respir J 17:259–267
Battisti A, Tassaux D, Janssens JP, Michotte JB, Jaber S, Jolliet P (2005) Performance characteristics of ten recent bilevel ventilators: a comparative bench study. Chest 127:1784–1792
Tassaux D, Strasser S, Fonseca S, Dalmas E, Jolliet P (2002) Comparative bench study of triggering, pressurization and cycling between the home ventilator VPAPII® and three ICU ventilators. Intensive Care Med 28:1254–1261
Richard JC, Carlucci A, Breton L, Langlais N, Jaber S, Maggiore S, Fougere S, Harf A, Brochard L (2002) Bench testing of pressure support ventilation with three different generations of ventilators. Intensive Care Med 28:1049–1057
Aslanian P, El Atrous S, Isabey D, Valente E, Corsi D, Harf A, Lemaire F, Brochard L (1998) Effects of flow triggering on breathing effort during partial ventilatory support. Am J Respir Crit Care Med 157:135–143
Nava S, Bruschi C, Rubini F, Palo A, Iotti G, Braschi A (1995) Respiratory response and inspiratory effort during pressure support ventilation in COPD patients. Intensive Care Med 21:871–879
Tassaux D, Michotte JB, Gainnier M, Gratadour P, Fonseca S, Jolliet P (2004) Expiratory trigger setting in pressure Support Ventilation: from mathematical model to bedside. Crit Care Med 32:1844–1850
Tassaux D, Gainnier M, Battisti A, Jolliet P (2005) Impact of expiratory trigger setting on delayed cycling and inspiratory muscle workload. Am J Respir Crit Care Med 172:1283–1289
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Vignaux, L., Tassaux, D. & Jolliet, P. Performance of noninvasive ventilation modes on ICU ventilators during pressure support: a bench model study . Intensive Care Med 33, 1444–1451 (2007). https://doi.org/10.1007/s00134-007-0713-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0713-0