Abstract
A gathering body of evidence has repeatedly revealed associations between indoor fungi and initiation, promotion, and exacerbation of allergic respiratory disease. The relationship between the exposure and outcome are complicated by the difficulties in measuring both exposure and outcome, the multifactorial nature of the disease, and the wide range of potential confounders. New technologies are becoming available that may enable better measurement of exposure and tighter case definitions so as to build more confidence in the associations discovered. The growing strength of the evidence base will aid the design of future public health interventions and generate new hypotheses on the cause of the rapid increase in allergic respiratory disease prevalence.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hill DJ, Munro DA, West PJ, Knox RB, Weston RH. Asthma in Melbourne children. Med J Aust. 1978;1:614–5.
Pepys J. Allergenic hypersensitivity to fungi. Postgraduate J Med. 1959;35:436–40.
Crameri R, Garbani M, Rhyner C, Huitema C. Fungi: the neglected allergenic sources. Allergy. 2014;69:176–85.
Arundel AV, Sterling EM, Biggin JH, Sterling TD. Indirect health effects of relative humidity in indoor environments. Environ Health Perspect. 1986;65:351–61.
Asher M, Montefort S, Björkstén B, Lai CKW, Strachan DP, Weiland SK, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC phases one and three repeat multicountry cross-sectional surveys. Lancet. 2006;368:733–43.
Terr AI. Are indoor molds causing a new disease? J Allergy Clin Immunol. 2004;113:221–6.
Jacobs J, Borràs-Santos A, Krop E, Täubel M, Leppänen H, Haverinen-Shaughnessy U, et al. Dampness, bacterial and fungal components in dust in primary schools and respiratory health in schoolchildren across Europe. Occup Environ Med. 2014;71:704–12.
Wilkins K, Nielsen K, Din S. Patterns of volatile metabolites and nonvolatile trichothecenes produced by isolates of stachybotrys, Fusarium, Trichoderma, trichothecium and memnoniella. Environ Sci Pollut Res. 2003;10:162–6.
O'Driscoll BR, Powell G, Chew F, Niven RM, Miles JF, Vyas A, et al. Comparison of skin prick tests with specific serum immunoglobulin E in the diagnosis of fungal sensitization in patients with severe asthma. Clin Exp Allergy. 2009;39:1677–83.
Smith M, Jäger S, Berger U, Šikoparija B, Hallsdottir M, Sauliene I, et al. Geographic and temporal variations in pollen exposure across Europe. Allergy. 2014;69:913–23.
Burge HA. An update on pollen and fungal spore aerobiology. J Allergy Clin Immunol. 2002;110:544–52.
Vesper S, McKinstry C, Haugland R, Wymer L, Bradham K, Ashley P, et al. Development of an environmental relative moldiness index for US homes. J Occup Environ Med. 2007;49:829–33.
Vesper SJ et al. Comparison of populations of mould species in homes in the UK and USA using mould-specific quantitative PCR. Appl Microbiol. 2005;41:367–73.
Vesper S, Wakefield J, Ashley P, Cox D, Dewalt G, Friedman W. Geographic distribution of environmental relative moldiness index molds in USA homes. J Environ Public Health. 2011;2011:11.
Anderson GP. Endotyping asthma: new insights into key pathogenic mechanisms in a complex, heterogeneous disease. Lancet. 2008;372:1107–19.
Lötvall J, Akdis CA, Bacharier LB, Bjermer L, Casale TB, Custovic A, et al. Asthma endotypes: a new approach to classification of disease entities within the asthma syndrome. J Allergy Clin Immunol. 2011;127:355–60.
Jacobsen EA, Lee NA, Lee JJ. Re-defining the unique roles for eosinophils in allergic respiratory inflammation. Clin Exp Allergy. 2014;44:1119–36.
Casas L, Tischer C, Wouters IM, Torrent M, Gehring U, Garcia-Esteban R, et al. Early life microbial exposure and fractional exhaled nitric oxide in school-age children: a prospective birth cohort study. Environ Heal. 2013;12:103.
Sachs-Olsen C, Lødrup Carlsen KC, Mowinckel P, Håland G, Devulapalli CS, Munthe-Kaas MC, et al. Diagnostic value of exhaled nitric oxide in childhood asthma and allergy. Pediatr Allergy Immunol. 2010;21:e213–21.
Blackwell M. The fungi: 1, 2, 3 … 5.1 million species? Am J Bot. 2011;98:426–38.
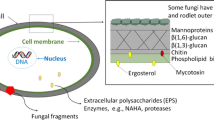
Thornton CR, Wills OE. Immunodetection of fungal and oomycete pathogens: established and emerging threats to human health, animal welfare and global food security. Crit Rev Microbiol. 2015;41:27–51.
Davies GE, Thornton CR. Differentiation of the emerging human pathogens trichosporon asahii and trichosporon asteroides from other pathogenic yeasts and moulds by using species-specific monoclonal antibodies. Plos One. 2014;9(1):e84789.
Miyagawa T, Hamagami S, Tanigawa N. Cryptococcus albidus-induced summer-type hypersensitivity pneumonitis. Am J Respir Crit Care Med. 2000;161:961–6.
Thornton CR. Breaking the mould—novel diagnostic and therapeutic strategies for invasive pulmonary aspergillosis in the immune deficient patient. Expert Rev Clin Immunol. 2014;10:771–80.
Brown GD, Denning DW, Gow NAR, Levitz SM, Netea MG, White TC. Hidden killers: human fungal infections. Sci Transl Med. 2012;4(165):165rv13.
Prattes J, Flick H, Prueler F, Koidi C, Raggam RB, Palfner M, et al. Novel tests for diagnosis of invasive Aspergillosis in patients with underlying respiratory diseases. Am J Respir Crit Care Med. 2014;190:922–9.
Huerta A, Soler N, Esperatti M, Guerrero M, Menendez R, Gimeno A, et al. Importance of aspergillus spp. Isolation in acute exacerbations of severe COPD: prevalence, factors and follow-up: the FUNGI-COPD study. Respir Res. 2014;15:17.
Thornton CR. Tracking the emerging human pathogen pseudallescheria boydii by using highly specific monoclonal antibodies. Clin Vaccine Immunol. 2009;16:756–64.
Thornton CR, Ryder LS, Le Cocq K, Soanes DM. Identifying the emerging human pathogen Scedosporium prolificans by using a species-specific monoclonal antibody that binds to the melanin biosynthetic enzyme tetrahydroxynaphthalene reductase. Environ Microbiol. 2015;17:1023–38.
Barton RC, Borman AM, Johnson EM, Houbraken J, Hobson RP, Denton M, et al. Isolation of the fungus geosmithia argillacea in sputum of people with cystic fibrosis. J Clin Microbiol. 2010;48:2615–7.
Nagano Y, Millar BC, Johnson E, Goldsmith CE, Elborn JS, Rendall J, et al. Fungal infections in patients with cystic fibrosis. Rev Med Microbiol. 2007;18:11–6.
Denning DW, O'Driscoll BR, Hogaboam CM, Bowyer P, Niven RM. The link between fungi and severe asthma: a summary of the evidence. Eur Respir J. 2006;27:615–26.
Denning DW, Pleuvry A, Cole DC. Global burden of allergic bronchopulmonary aspergillosis with asthma and its complication chronic pulmonary aspergillosis in adults. Med Mycol. 2013;51:361–70.
Knutsen AP, Slavin RG. Allergic bronchopulmonary aspergillosis in asthma and cystic fibrosis. Clin Dev Immunol 2011; 2011:843763.
Kurup VP. Aspergillus antigens: which are important? Med Mycol. 2005;43:S189–96.
De Hoog GS, Queiroz-Telles F, Haase G, Fernandez-Zeppenfeldt G, Angelis DA, Van den Ende AHGG, et al. Black fungi: clinical and pathogenic approaches. Med Mycol. 2000;38:243–50.
Chou H, Tam MF, Lee LH, Chiang CH, Tai HY, Panzani RC, et al. Vacuolar serine protease is a major allergen of cladosporium cladosporioides. Int Arch Allergy Immunol. 2008;146:277–86.
Vojdani A. Antibodies against Stachybotrys chartarum extract and its antigenic components, stachyhemolysin and stachyrase-A: a new clinical biomarker. Med Sci Monit. 2005;11:BR139–45.
Wartenberg D, Lapp K, Jacobsen ID, Dahse H-M, Kniemeyer O, Heinekamp T, et al. Secretome analysis of aspergillus fumigatus reveals Asp-hemolysin as a major secreted protein. Int J Med Microbiol. 2011;301:602–11.
Pringle A. Asthma and the diversity of fungal spores in air. PLoS Pathog. 2013;9:e1003371.
Sharpe RA, Bearman N, Thornton CR, Husk K, Osborne NJ. Indoor fungal diversity and asthma: a meta-analysis and systematic review of risk factors. J Allergy Clin Immunol. 2014;135:110–22. First systematic review and meta-analysis on the diversity and concentrations of indoor fungi, which highlights a number of limitations with the inconsistency and difficulty in assessing the role of indoor fungal species on health.
Quansah R, Jaakkola MS, Hugg TT, Heikkinen SAM, Jaakkola JJK. Residential dampness and molds and the risk of developing asthma: a 7-12 july 2014 systematic review and meta-analysis. PLoS ONE. 2012;7:e47526. Builds on the reviews of Fisk and Mendell and is the first to implicate exposure to fungi and risk of developing allergic diseases.
Fisk WJ, Lei-Gomez Q, Mendell MJ. Meta-analyses of the associations of respiratory health effects with dampness and mold in homes. Indoor Air. 2007;17:284–96.
Nevalainen A, Täubel M, Hyvärinen A. Indoor fungi: companions and contaminants. Indoor Air. 2015;25:125–56.
Sharpe R, Thornton CR, Osborne NJ. Modifiable factors governing indoor fungal diversity and risk of asthma. Clin Exp Allergy. 2014;44:631–41.
Barberán A, Dunn RR, Reich BJ, Pacifici K, Laber EB, Menninger HL, et al. The ecology of microscopic life in household dust. Proc R Soc Lond B Biol Sci 2015; 282.
Méheust D, Le Cann P, Reboux G, Millon L, Gangneux J-P. Indoor fungal contamination: health risks and measurement methods in hospitals, homes and workplaces. Crit Rev Microbiol. 2013;0:1–13.
Frankel M, Bekö G, Timm M, Gustavsen S, Hansen EW, Madsen AM. Seasonal variations of indoor microbial exposures and their relation to temperature, relative humidity, and Air exchange rate. Appl Environ Microbiol. 2012;78:8289–97.
Johansson P, Bok G, Ekstrand-Tobin A. The effect of cyclic moisture and temperature on mould growth on wood compared to steady state conditions. Build Environ. 2013;65:178–84.
Mensah-Attipoe J, Reponen T, Salmela A, Veijalainen A-M, Pasanen P. Susceptibility of green and conventional building materials to microbial growth. Indoor Air 2014:(accepted).
Andersen B, Frisvad JC, Søndergaard I, Rasmussen IS, Larsen LS. Associations between fungal species and water-damaged building materials. Appl Environ Microbiol. 2011;77:4180–8.
Verdier T, Coutand M, Bertron A, Roques C. A review of indoor microbial growth across building materials and sampling and analysis methods. Build Environ. 2014;80:136–49.
Flannigan B, Samson RA, Miller JD. Microorganisms in home and indoor work environments - diversity, health impacts, investigation and control. 2nd ed. Florida: CRC Press; 2011.
Reponen T, Singh U, Schaffer C, Vesper S, Johansson E, Adhikari A, et al. Visually observed mold and moldy odor versus quantitatively measured microbial exposure in homes. Sci Total Environ. 2010;408:5565–74.
Haverinen-Shaughnessy U. Prevalence of dampness and mold in European housing stock. J Expo Sci Environ Epidemiol. 2012;22:461–7.
Sharpe RA, Thornton CR, Nikolaou V, Osborne NJ. Fuel poverty increases risk of mould contamination, regardless of adult risk perception & ventilation in social housing properties. Environ Int. 2015;79:115–29.
Frankel M, Hansen EW, Madsen AM. Effect of relative humidity on the aerosolization and total inflammatory potential of fungal particles from dust-inoculated gypsum boards. Indoor Air. 2014;24:16–28.
Seo S, Choung JT, Chen BT, Lindsley WG, Kim KY. The level of submicron fungal fragments in homes with asthmatic children. Environ Res. 2014;131:71–6.
Sharpe RA, Thornton CR, Nikolaou V, Osborne NJ. Higher energy efficient homes are associated with increased risk of doctor diagnosed asthma in a UK sub population. Environ Int. 2015;75:234–44.
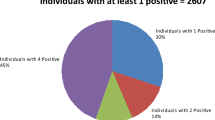
Sharpe RA, Thornton CR, Tyrrell J, Nikolaou V, Osborne NJ. Variable risk of atopic disease due to indoor fungal exposure in NHANES 2005–2006. Clin Exp Allergy. 2015;45:1566–78. Highlights the complexity of investigating indoor fungi and interaction with the indoor microbiome, but also the role of allergic and non-allergic mechanisms.
Hernberg S, Sripaiboonkij P, Quansah R, Jaakkola JK, Jaakkola MS. Indoor molds and lung function in healthy adults. Respir Med. 2014;108:677–84. Demonstrates the inflammatory potential in healthy populations.
Larsson M, Hägerhed-Engman L, Moniruzzaman S, Janson S, Sundell J, Bornehag C-G. Can we trust cross-sectional studies when studying the risk of moisture-related problems indoor for asthma in children? Int J Environ Health Res. 2011;21:237–47.
Hägerhed-Engman L, Sigsgaard T, Samuelson I, Sundell J, Janson S, Bornehag CG. Low home ventilation rate in combination with moldy odor from the building structure increase the risk for allergic symptoms in children. Indoor Air. 2009;19:184–92.
Vesper S, Barnes C, Ciaccio CE, Johanns A, Kennedy K, Murphy JS, et al. Higher environmental relative moldiness index (ERMI) values measured in homes of asthmatic children in Boston, Kansas city, and San Diego. J Asthma. 2013;50(2):155–61.
Vesper SJ, Wymer L, Kennedy S, Grimsley LF. Decreased pulmonary function measured in children exposed to high environmental relative moldiness index homes. Open Respir Med J. 2013;7:83–6.
Reponen T, Lockey J, Bernstein DI, Vesper SJ, Levin L, Hershey GKK, et al. Infant origins of childhood asthma associated with specific molds. J Allergy Clin Immunol. 2012;130:639–44. Use of the ERMI and identification of key indoor species associated with new asthma symptoms, highlighting the potential for this technique to assess indoor exposures.
Méheust D, Le Cann P, Reponen T, Wakefield J, Vesper S, Gangneux J-P. Possible application of the environmental relative moldiness index in France: a pilot study in Brittany. Int J Hyg Environ Health. 2013;216:333–40.
McSharry C, Vesper S, Wymer L, Howieson S, Chaudhuri R, Wright GR, et al. Decreased FEV1% in asthmatic adults in Scottish homes with high environmental relative moldiness index values. ClinExp Allergy. 2015;45:902–7.
Vesper SJ, McKinstry C, Haugland RA, Iossifova Y, Lemasters G, Levin L, et al. Relative moldiness index as predictor of childhood respiratory illness. J Expo Sci Environ Epidemiol. 2006;17:88–94.
Pitkäranta M, Meklin T, Hyvärinen A, Nevalainen A, Paulin L, Auvinen P, et al. Molecular profiling of fungal communities in moisture damaged buildings before and after remediation—a comparison of culture-dependent and culture-independent methods. BMC Microbiol. 2011;11:235.
Mendell MJ, Mirer AG, Cheung K, Tong M, Douwes J. Respiratory and allergic health effects of dampness, mold, and dampness-related agents: a review of the epidemiologic evidence. Environ Health Perspect. 2011;119:748–56.
Mendall M. Indoor dampness and mold as indicators of respiratory health risks, part 2: a brief update on the epidemiologic evidence. 13th International Conference on Indoor Air Quality and Climate 2014 Hong Kong, 2014.
Antova T, Pattenden S, Brunekreef B, Heinrich J, Rudnai P, Forastiere F, et al. Exposure to indoor mould and children’s respiratory health in the PATY study. J Epidemiol Community Health. 2008;62:708–14.
Tischer CG, Hohmann C, Thiering E, Herbarth O, Müller A, Henderson J, et al. Meta-analysis of mould and dampness exposure on asthma and allergy in eight European birth cohorts: an ENRIECO initiative. Allergy. 2011;66:1570–9. Examined relationship between fungi and dampness and asthma and allergy across a range of populations.
Sharpe RA, Bearman N, Thornton CR, Husk K, Osborne NJ. Indoor fungal diversity and asthma: a meta-analysis and systematic review of risk factors. J Allergy Clin Immunol. 2015;135:110–22.
Matheson MC, Abramson MJ, Dharmage SC, Forbes AB, Raven JM, Thien FCK, et al. Changes in indoor allergen and fungal levels predict changes in asthma activity among young adults. Clin Exp Allergy. 2005;35:907–13.
Das P, Chalabi Z, Jones B, Milner J, Shrubsole C, Davies M, et al. Multi-objective methods for determining optimal ventilation rates in dwellings. Build Environ. 2013;66:72–81.
BSI. Code of practice for control of condensation in buildings. BS 5250:2011. UK: British Standards Institute, 2011.
Simon-Nobbe B, Denk U, Pöll V, Rid R, Breitenbach M. The spectrum of fungal allergy. Int Arch Allergy Immunol. 2008;145:58–86.
Wilkinson P, Smith KR, Beevers S, Tonne C, Oreszczyn T. Energy, energy efficiency, and the built environment. Lancet. 2007;370:1175–87.
Twaroch TE, Curin M, Valenta R, Swoboda I. Mold allergens in respiratory allergy: from structure to therapy. Allergy Asthma Immunol Res. 2015;7:205–20.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Drs. Osborne, Thornton, and Sharpe declare that they have no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Allergens
Rights and permissions
About this article
Cite this article
Osborne, N.J., Thornton, C.R. & Sharpe, R.A. Indoor Fungal Exposure and Allergic Respiratory Disease. Curr Allergy Asthma Rep 15, 71 (2015). https://doi.org/10.1007/s11882-015-0572-7
Published:
DOI: https://doi.org/10.1007/s11882-015-0572-7