Abstract
Purpose
The purpose of this study was to evaluate altered pulmonary function retrospectively after RFA.
Methods
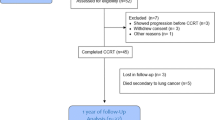
This retrospective study comprised 41 ablation sessions for 39 patients (22 men and 17 women; mean age, 64.8 years). Vital capacity (VC) and forced expiratory volume in 1 s (FEV1) at 1 and 3 months after RFA were compared with the baseline (i.e., values before RFA). To evaluate the factors that influenced impaired pulmonary function, univariate analysis was performed by using multiple variables. If two or more variables were indicated as statistically significant by univariate analysis, these variables were subjected to multivariate analysis to identify independent factors.
Results
The mean VC and FEV1 before RFA and 1 and 3 months after RFA were 3.04 and 2.24 l, 2.79 and 2.11 l, and 2.85 and 2.13 l, respectively. The values at 1 and 3 months were significantly lower than the baseline. Severe pleuritis after RFA was identified as the independent factor influencing impaired VC at 1 month (P = 0.003). For impaired FEV1 at 1 month, only severe pleuritis (P = 0.01) was statistically significant by univariate analysis. At 3 months, severe pleuritis (VC, P = 0.019; FEV1, P = 0.003) and an ablated parenchymal volume ≥20 cm3 (VC, P = 0.047; FEV1, P = 0.038) were independent factors for impaired VC and FEV1.
Conclusions
Pulmonary function decreased after RFA. RFA-induced severe pleuritis and ablation of a large volume of marginal parenchyma were associated with impaired pulmonary function.

Similar content being viewed by others
References
Pennathur A, Luketich JD, Abbas G et al (2007) Radiofrequency ablation for the treatment of stage I non-small cell lung cancer in high-risk patients. J Thorac Cardiovasc Surg 134:857–864
Lencioni R, Crocetti L, Cioni R et al (2008) Response to radiofrequency ablation of pulmonary tumours: a prospective, intention-to-treat, multicenter clinical trial (the RAPTURE study). Lancet Oncol 9:621–628
Hiraki T, Gobara H, Iishi T et al (2007) Percutaneous radiofrequency ablation for clinical stage I non-small cell lung cancer: results in 20 nonsurgical candidates. J Thorac Cardiovasc Surg 134:1306–1312
Yan TD, King J, Sjarif A et al (2006) Percutaneous radiofrequency ablation of pulmonary metastases from colorectal carcinoma: prognostic determinants for survival. Ann Surg Oncol 13:1529–1537
Hiraki T, Gobara H, Iishi T et al (2007) Percutaneous radiofrequency ablation for pulmonary metastases from colorectal cancer: midterm results in 27 patients. J Vasc Interv Radiol 18:1264–1269
Yamakado K, Hase S, Matsuoka T et al (2007) Radiofrequency ablation for the treatment of unresectable lung metastases in patients with colorectal cancer: a multicenter study in Japan. J Vasc Interv Radiol 18:393–398
Hiraki T, Tajiri N, Mimura H et al (2006) Pneumothorax, pleural effusion, and chest tube placement after radiofrequency ablation of lung tumors: incidence and risk factors. Radiology 241:275–283
Goldberg SN, Gazelle GS, Compton CC, McLoud TC (1995) Radiofrequency tissue ablation in the rabbit lung: efficacy and complications. Acad Radiol 2:776–784
Ambrogi MC, Lucchi M, Dini P et al (2006) Percutaneous radiofrequency ablation of lung tumors: results in mid-term. Eur J Cardiothorac Surg 30:177–183
de Baère T, Palussière J, Aupèrin A et al (2006) Midterm local efficacy and survival after radiofrequency ablation of lung tumors with minimum follow-up of 1 year: prospective evaluation. Radiology 240:587–596
Brunelli A, Xiumé F, Refai M et al (2007) Evaluation of expiratory volume, diffusion capacity, and exercise tolerance following major lung resection: a prospective follow-up analysis. Chest 131:141–147
Okada M, Koike T, Higashiyama M et al (2006) Radical sublober resection for small-sized non-small lung cancer: a multicenter study. J Thorac Cardiovasc Surg 132:769–775
Conflict of Interest
None.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Severe pleuritis and larger ablated parenchymal volume were the variables that were obtained after RFA. Thus, regrettably, those were not quite helpful in predicting impaired pulmonary function in advance. Then, additional analysis was performed to evaluate the predictive factors for the occurrence of severe pleuritis and larger ablated parenchymal volume. Univariate analysis with chi-square test or Fisher’s exact tests was performed by using multiple variables that were available before RFA, including age, sex, pulmonary emphysema, pre-RFA %VC, pre-RFA FEV1%, tumor type, distance to the nearest pleura from tumors, tumor volume, and electrode type. The results are shown in Table 5.
Although there was no variable significantly increasing a risk of severe pleuritis, pulmonary emphysema had a tendency (P = 0.052) to be associated with the occurrence of severe pleuritis after RFA. The variables that increased a risk of larger ablated parenchymal volume significantly were emphysema (P = 0.029) and tumor volume ≥1.3 cm3 (P = 0.011). Given that ventilation and perfusion has heat sink effect, decreased ventilation and perfusion in the emphysematous lung may explain the association between pulmonary emphysema and more extensive ablation leading to severe pleuritis and larger ablated parenchymal volume.
Rights and permissions
About this article
Cite this article
Tada, A., Hiraki, T., Iguchi, T. et al. Influence of Radiofrequency Ablation of Lung Cancer on Pulmonary Function. Cardiovasc Intervent Radiol 35, 860–867 (2012). https://doi.org/10.1007/s00270-011-0221-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-011-0221-z