Abstract
It has been suggested that activation of nuclear peroxisome proliferator-activated receptors γ (PPARγ) may represent a new strategy for the treatment of pulmonary arterial hypertension. It has been demonstrated that PPARγ activation relaxed the isolated mouse pulmonary artery. The aims of the present study were to examine whether and to which extent the two PPARγ agonists rosiglitazone and pioglitazone relax the isolated human pulmonary artery and to investigate the underlying mechanism(s). Isolated human pulmonary arteries were obtained from patients without clinical evidence of pulmonary hypertension during resection of lung carcinoma. Vasodilatory effects of PPARγ agonists were examined on endothelium-intact or endothelium-denuded vessels preconstricted with the thromboxane prostanoid receptor agonist U-46619. Rosiglitazone and pioglitazone (0.01–100 μM) caused a concentration- and/or time-dependent full relaxation of U-46619-preconstricted vessels. The rosiglitazone-induced relaxation was attenuated by the PPARγ antagonist GW9662 1 μM, endothelium denudation, the nitric oxide synthase inhibitor L-NAME 300 μM, the cyclooxygenase inhibitor indomethacin 10 μM, and the KATP channel blocker glibenclamide 10 μM. The prostacyclin IP receptor antagonist RO1138452 1 μM shifted the concentration–response curve for rosiglitazone to the right. The PPARγ agonists pioglitazone and rosiglitazone relax human pulmonary arteries. The rosiglitazone-induced vasorelaxation is partially endothelium-dependent and involves PPARγ receptors, arachidonic acid degradation products, nitric oxide, and KATP channels. Thus, the relaxant effect of PPARγ agonists in human pulmonary arteries may represent a new therapeutic target in pulmonary arterial hypertension.
Similar content being viewed by others
Introduction
Pulmonary arterial hypertension (PAH) is a disease characterized by increased pulmonary arterial pressure accompanied by an increase in pulmonary vascular resistance, by pulmonary vascular remodeling, and endothelial dysfunction leading to right ventricular failure and premature death. So far, the available therapies (including phosphodiesterase type 5 inhibitors, endothelin-1 receptor antagonists or prostacyclin mimetics) may help relieve symptoms and slow the progress of the disease but still PAH has no cure. Thus, there is an urgent need for novel and more effective therapeutic strategies in the PAH treatment. In recent years, evidence has been accumulating that activation of nuclear peroxisome proliferator-activated receptors γ (PPARγ) may be a novel, attractive PAH therapeutic target (for review, see, e.g., Sutliff et al. 2010; Archer et al. 2010; Green et al. 2011).
PPARγ receptors are normally expressed in human endothelial and smooth muscle cells of the pulmonary vascular wall (for review, see, e.g., Sutliff et al. 2010; Green et al. 2011). However, their expression was diminished in vascular lesions (both in smooth muscle and endothelial cells) from patients with primary and secondary pulmonary hypertension (Ameshima et al. 2003). Moreover, hypoxia decreased PPARγ expression in human pulmonary artery smooth muscle and endothelial cells (Lu et al. 2010; Nisbet et al. 2010). The above observations are further supported by experiments on animals. Thus, hypoxia induced severe PAH and decreased lung vascular PPARγ expression in mice (Gong et al. 2011) and in rats (Ameshima et al. 2003; Kim et al. 2010; Gong et al. 2011). Similarly, the PPARγ protein level in lung tissue was also diminished in a lamb model of increased pulmonary blood flow and PAH induced by an aorta-to-pulmonary artery shunt (Oishi et al. 2013).
From all PPARγ ligands, thiazolidinediones are of the most clinical importance. They are insulin sensitizers and are known because of their antidiabetic efficacy. Increasing evidence suggests that thiazolidinediones, in addition to improving glycemic control, cause vascular vasodilatation of systemic arteries and modestly lower blood pressure both in human and in animal insulin-resistant and non-insulin-resistant models of hypertension (for review, see, e.g., Sigmund 2010; Sutliff et al. 2010; Green et al. 2011; Salomone and Drago 2012). The representative members of thiazolidinediones and PPARγ agonists are rosiglitazone and pioglitazone. Rosiglitazone is one of the most potent and selective synthetic agonists of PPARγ receptors, and pioglitazone is the only thiazolidinedione currently approved for clinical practice in Europe (for reviews, see Michalik et al. 2006; Ciudin et al. 2012). Unfortunately, their effects on pulmonary circulation have been examined in few studies only. So, chronic rosiglitazone administration prevented the loss of agonist-induced endothelium-dependent vascular relaxation in the lamb model mentioned above (Oishi et al. 2013). It also attenuated the hypoxia-induced PAH in rats (Crossno et al. 2007; Kim et al. 2010) and in adult (but not in newborn) mice (Nisbet et al. 2010; Nicola et al. 2011). Moreover, it prevented PAH development in male apolipoprotein E-deficient (ApoE−/−) mice on a high-fat diet (Hansmann et al. 2007).
In other words, PPARγ agonists protect against PAH development in a series of experimental models and their beneficial effects may be connected, e.g., with the alteration of the balance between vasoconstrictor and vasodilator substances (for review, see Sutliff et al. 2010; Green et al. 2011; Salomone and Drago 2012). A direct vasodilatory effect of rosiglitazone in the isolated pulmonary artery has been so far shown in the mouse only (Harrington et al. 2010). Thus, the aim of the present study was to examine the vasodilator effect of rosiglitazone also in the human pulmonary artery (hPA) and to include pioglitazone, another representative member of PPARγ agonists. In addition, the involvement of PPARγ receptors, endothelium, arachidonic acid degradation products, nitric oxide, and KATP channels in the vasodilator effect of rosiglitazone was investigated.
Material and methods
In accordance with the Declaration of Helsinki, the study protocol was approved by the local ethics committee (No. R-I-002/309/2008), and written informed consent was obtained from all donors for the use of their tissue.
Tissue preparation
Human lung tissue was obtained from 44 patients (31 men and 13 women, mean age 66.5 ± 1.9 years) undergoing lobectomy or pneumonectomy during resection of lung carcinoma. Preoperative echocardiography revealed normal left and right ventricular function in each case. Patients did not have any clinical evidence of pulmonary hypertension nor did they receive beta-blockers. Before the operation, all patients received cephalosporins and low molecular weight heparin as anti-infection and anti-thrombotic prophylaxis, respectively. The tissue was transported to the laboratory within half an hour in cold (4 °C), pre-gassed Tyrode’s bicarbonate solution (for composition, see below). Lobar and segmental branches of the hPA were cleaned from the lung parenchyma and cut into rings (from the middle portion of each artery; 3–5 mm length and 2–4 mm outer diameter).
Organ bath technique
The arterial rings were suspended on stainless steel wires in 10 ml organ baths containing Tyrode’s solution (concentration in mM: NaCl, 139.2; KCl, 2.7; CaCl2, 1.8; MgCl2, 0.49; NaHCO3, 11.9; NaH2PO4, 0.4; glucose, 5.5) and were gassed continuously with 95 % O2 and 5 % CO2, at 37 °C and pH 7.4. Pulmonary artery rings were allowed to equilibrate for 90 min; during this time period, the bath fluid was exchanged every 10 min with fresh Tyrode’s solution. The optimal resting tension was about 20–25 mN (depending on the rings’ internal diameter), which ensured that responses to agonists were maximal. Muscle tension was recorded by a force displacement transducer (PIM 100RE, BIO-SYS-TECH, Białystok, Poland) and displayed on a computer.
After the equilibration period, all rings were preconstricted submaximally with phenylephrine (1 μM) to prime the tissues and to check the functionality of the endothelium (at least 80 % relaxation in response to acetylcholine 1 μM). For experiments with endothelium-free vascular wall, vessels were denuded by rubbing the intimal surface mechanically, and successful endothelial removal was confirmed by a lack of vasorelaxant response to acetylcholine. Viable vessels were constricted submaximally with U-46619 (a thromboxane prostanoid receptor agonist). Since the degree of relaxation crucially depends on the level of the tone of the tissue (Guimarães and Moura 2001), the concentration of U-46619 was titrated within a range of 0.01–0.03 μM to achieve a comparable contraction level for each group when compared to the respective control group. When a stable level of tone was maintained (after about 45 min exposure time), the vasorelaxant effects of the agonists were examined. Rosiglitazone was given in two ways. In the first series, only one concentration of the agonist (0.1, 1, 10, and 100 μM) was administered in one arterial preparation in order to examine its time-dependent effect, and the relaxant influence of agonist was observed over 120 min. To assess the contribution of PPARγ activation, some experiments were performed in the presence of the PPARγ antagonist GW9662 (1 or 10 μM; O’Sullivan et al. 2005, 2006) added 10 min prior to precontraction (O’Sullivan et al. 2005). In the second series, cumulative concentration–response curves (CRCs) for rosiglitazone and pioglitazone (0.01–100 μM) or the prostacyclin (IP) receptor agonist iloprost (0.001–10 μM) were constructed by cumulative addition of agonists in order to examine their vasodilatory effects. In order to examine the mechanism(s) involved in the vasodilatory effect of the agonists, rings were exposed from 30 min prior to precontraction of arteries until the end of the experiments with the following inhibitors (the respective receptors, enzymes, or ion channels are given in brackets): RO1138452 1 and 10 μM (prostacyclin IP receptors; Jones et al. 2006), N G-nitro-l-arginine methyl ester (L-NAME) 300 μM (nitric oxide synthase; Kozłowska et al. 2007), indomethacin 10 μM (cyclooxygenase, COX; Kozłowska et al. 2007), and glibenclamide 10 μM (KATP; Irat et al. 2006). In control tissues of both series, the respective vehicle of agonists or antagonists was used instead. In each individual preparation, only one experimental curve was determined. All experiments were performed in paired vessels, i.e., the effect of a drug or of endothelium denudation was studied in one vessel, whereas another vessel from the same patient served as control.
In order to examine whether rosiglitazone is a direct antagonist at the thromboxane receptor, some rings were treated for 30 min with one concentration (10 μM) of rosiglitazone or its vehicle (DMSO 0.01 % v/v; controls) and then the CRC for U-46619 (0.001–3 μM) was constructed.
Drugs used
(−)-Phenylephrine hydrochloride, acetylcholine chloride, and L-NAME (Sigma, Munich, Germany) were dissolved in deionized water, whereas indomethacin (Sigma, Munich, Germany) was dissolved in 0.5 M NaHCO3. Iloprost (Schering AG, Berlin, Germany) was dissolved in 0.9 % NaCl. U-46619 (9,11-dideoxy-9α,11α-methanoepoxy prostaglandin F2α) (Cayman Chemicals, Ann Arbor, MI, USA) was supplied in 100 % ethanol and further diluted with deionized water to the concentration required. Rosiglitazone (Cayman Chemicals) and pioglitazone hydrochloride (Biotrend, Köln, Germany) were supplied in DMSO and further diluted with deionized water to the concentration required. Stock solutions of glibenclamide (in DMSO) and RO1138452 (4,5-dihydro-N-[[4-(1-methylethoxy)phenyl)]-1H-imidazol-2-amine, CAY-10441) (Cayman Chemicals) (in ethanol) were diluted with water such that the final concentration of the organic solvent in the organ bath was less than 0.01 % v/v.
Calculations and statistical analysis
The relaxation elicited by rosiglitazone, pioglitazone, and iloprost or their solvents was expressed as percentage of the precontraction induced by U-46619. EC50 values were used to determine the potency of U-46619 as a contractile agent and of rosiglitazone and iloprost as vasodilators. For U-46619, the EC50 is the concentration causing the half-maximum effect, and for rosiglitazone and iloprost, the EC50 is the concentration causing a relaxation of 50 % of the precontracted vessel. Note that for rosiglitazone, EC50 values could be obtained only for those experiments in which one concentration was given per vessel, since in the experiments with cumulative administration, plateaus of the vasodilatory effect were not reached when the next higher drug concentrations were given. The antagonistic potency (pA2) of RO1138452 against iloprost was calculated from the equation pA2 = −log[B] + log (r − 1), where [B] is the molar concentration of RO1138452 and r is the concentration ratio of the EC50 values of iloprost in the presence and absence of RO1138452. In order to assess the potency of endothelial denudation and of various antagonists and inhibitors in those experiments in which rosiglitazone was given cumulatively, the rightward shift was determined on the basis of the EC25 values, i.e., those values leading to a vasodilation of 25 % of the precontracted vessel.
Results are expressed as mean ± SEM of n experiments from three different patients (data from Figs. 1 and 5b) and from at least four different patients (rest). Statistical analyses were performed using t test for unpaired data. When two or more treatment groups were compared to the same control, the one-way analysis of variance followed by the Dunnett test was used (Prism 5, GraphPad Software Inc., La Jolla, CA, USA). Differences were considered as significant when P < 0.05.
Influence of rosiglitazone on the concentration-dependent vasocontraction induced by U-46619 in endothelium-intact human pulmonary arteries. Results are expressed as percentage of maximal (max.) contraction. Mean ± SEM of three arteries for each curve. In many cases, SEM is smaller than or equal to the size of symbols
Results
General
The vasodilatory effect of rosiglitazone was studied under various experimental conditions. The thromboxane A2 receptor agonist U-46619 was used to precontract the hPA. U-46619 (0.001–3 μM) induced a virtually identical concentration-dependent contraction in the absence (pEC50 = 7.54 ± 0.04, n = 3) and in the presence of rosiglitazone (10 μM; pEC50 = 7.43 ± 0.06, n = 3) (Fig. 1). Rosiglitazone did not modify the basal tone by itself (not shown). In the subsequent experiments, the vascular rings were first preconstricted with U-46619 at a concentration approximately equivalent to its EC60.
In preparatory experiments, the U-46619-induced contraction was not affected by GW9662 (1 and 10 μM), RO1138452 (1 and 10 μM), and endothelial denudation but slightly increased by L-NAME (300 μM), indomethacin (10 μM), and glibenclamide (10 μM) (not shown). To adjust the degree of the U-46619-induced contraction to the level in controls, lower concentrations of U-46619 were used in the presence of the latter three inhibitors (for details, see “Material and methods”). In this way, the tension, which amounted to 8.92 ± 0.98 in 17 controls, did not differ between the various experimental groups (not shown).
Vasodilatory effects of PPARγ agonists
As shown in Fig. 2a, pioglitazone and rosiglitazone (0.01–100 μM each) given cumulatively caused a concentration-dependent full relaxation of the endothelium-intact hPAs preconstricted with U-46619. The first vasodilatory effect of pioglitazone and rosiglitazone (by about 20 %) was induced by 3 and 1 μM, respectively, and occurred about 25–30 min after the administration of the lowest concentration of the agonist. The time necessary to reach full vasorelaxation was 100.9 ± 6.4 (n = 8) and 102.3 ± 7.2 min (n = 17), respectively. Rosiglitazone exhibited a slightly greater potency than pioglitazone (by a factor of 2.1). Thus, in all further studies, we examined the vasodilatory effect of rosiglitazone only.
Concentration–response curves (a) and representative original traces (b, c) of the rosiglitazone- and/or pioglitazone-induced relaxation of endothelium-intact isolated human pulmonary arteries. A cumulative concentration–response curve was constructed [pioglitazone (a) or rosiglitazone (a, c)] or single concentrations of rosiglitazone were given (a, b; exposure time 120 min). Arrows (b, c) show the moment of application of the particular concentrations of rosiglitazone. Broken arrows (c) represent the following concentrations (from the left): 0.03, 0.3, 3, and 30 μM, respectively. Results in a are expressed as percentage relaxation of the isometric contraction induced by U-46619. Mean ± SEM of 5–17 tissues for each curve
Rosiglitazone, given in single concentrations, (but not its vehicle) caused not only a concentration- but also time-dependent relaxation of the endothelium-intact hPAs preconstricted with U-46619 (Figs. 2 and 3). The shape of the time–effect curves suggests that the maximal relaxation obtainable with each of the four concentrations of rosiglitazone occurs after about 120 min. A virtually full relaxation was obtained with the highest concentration of rosiglitazone. The pEC50 value was 5.55 (n = 6–10; points for particular concentrations were obtained from different patients, and for this reason, an SEM value could not be determined). A comparison of the CRCs for rosiglitazone given cumulatively and separately shows that they are very similar (Fig. 2a).
Time-dependent vasorelaxation induced by single concentrations of rosiglitazone (a) and its interaction with the PPARγ receptor antagonist GW9662 (b) in the human endothelium-intact pulmonary artery. Results are expressed as percentage relaxation of the isometric contraction induced by U-46619. Mean ± SEM of five to ten tissues for each curve. *P < 0.05, **P < 0.01, ***P < 0.001 compared to rosiglitazone alone
Involvement of PPARγ receptors in the vasodilatory effect of rosiglitazone
The PPARγ antagonist GW9662 (1 and 10 μM) reduced the time-dependent relaxation induced by rosiglitazone (10 μM; approximately equivalent to its EC70) in a concentration-dependent manner. The attenuation became significant after 60 and 30 min, and the maximal effects (at 120 min) were diminished by about 35 and 80 %, respectively (Fig. 3b).
Involvement of NO, cyclooxygenase product(s), and KATP channels in the vasodilatory effect of rosiglitazone
The CRC for rosiglitazone (given cumulatively) was shifted to the right by removal of the endothelium, the cyclooxygenase inhibitor indomethacin (10 μM), and the inhibitor of NO synthesis, L-NAME (300 μM), by factors of 10, 13, and 10, respectively. Under each condition, the relaxation obtained with the highest agonist concentration was diminished by about 50 % (Fig. 4a, b). The KATP channel antagonist glibenclamide (10 μM) diminished the rosiglitazone (100 μM)-induced relaxation by about 70 % and shifted its CRC to the right by a factor of 35 (Fig. 4a). The vehicle for glibenclamide (DMSO 0.01 % v/v) did not modify the CRC for rosiglitazone (not shown).
Influence of endothelium removal, of the KATP channel blocker glibenclamide (a), the NO synthesis inhibitor N G-nitro-l-arginine methyl ester (L-NAME), and the cyclooxygenase inhibitor indomethacin (Indo) (b) on the concentration-dependent vasorelaxation induced by rosiglitazone in human pulmonary arteries. Results are expressed as percentage relaxation of the isometric contraction induced by U-46619. In a, the effect of the vehicle for rosiglitazone (DMSO 0.01 % v/v each) is shown as well. Mean ± SEM of 7–17 tissues for each curve
Involvement of IP receptors in the vasodilatory effect of rosiglitazone
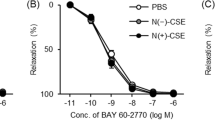
The prostacyclin IP receptor antagonist RO1138452 (1 and 10 μM) reduced the rosiglitazone (100 μM)-induced vasodilation by about 50 and 85 %, respectively (Fig. 5a). The lower concentration of RO1138452 shifted the CRC for rosiglitazone to the right by a factor of 13 (Fig. 5a).
Influence of the prostacyclin IP receptor antagonist RO1138452 on the concentration-dependent vasorelaxation induced by rosiglitazone (a) and iloprost (b) in human endothelium-intact pulmonary arteries. Results are expressed as percentage relaxation of the isometric contraction induced by U-46619. Mean ± SEM of three to seven tissues for each curve
In additional experiments, the interaction of RO1138452 with the stable analogue of prostacyclin, iloprost, was studied as well (Fig. 5b). Iloprost (0.001–10 μM) caused a full relaxation of the endothelium-intact hPA preconstricted with U-46619. Although the lower part of the CRC may suggest a biphasic effect, evaluation with a computer-based fitting program revealed that a monotonic curve is statistically preferred. RO1138452 (1 μM) attenuated the iloprost (10 μM) relaxation by 30 % and shifted the CRC for iloprost to the right by a factor of 14. Since for iloprost (as opposed to rosiglitazone) the vasodilator effects upon cumulative administration plateaued within short time periods, pEC50 and apparent pA2 values could be determined. The pEC50 for iloprost (in the absence of RO1138452) is 6.47 ± 0.22 and the apparent pA2 of RO1138452 (1 μM) against iloprost is 7.21.
Discussion
The aim of the present study was to examine whether PPARγ agonists influence the contractile tone of the human pulmonary artery and we could show for the first time that both rosiglitazone and pioglitazone relax this vessel. In addition, the potential mechanisms involved in the vasodilator effect of rosiglitazone were studied. For the experiments, we used the thromboxane analogue U-46619 as the contractile agent since thromboxane A2 plays a major role as a vasoconstrictor in the pulmonary circulation and may be involved in the pathogenesis of pulmonary hypertension (for review, see Sutliff et al. 2010; Archer et al. 2010; Green et al. 2011). In addition, U-46619 was also used in most other studies in which vasodilator effects of PPARγ agonists were examined (see below). The possibility had to be considered that the vasorelaxant effect of rosiglitazone in our model, like in mouse mesenteric arteries (Yuen et al. 2011), is related to a direct antagonistic effect at thromboxane (TP) receptors, but rosiglitazone 10 μM (i.e., at a concentration which relaxes the hPA preconstricted with U-46619 by 60–70 %) did not modify the U-46619-induced vasoconstriction in pulmonary arteries without preconstriction. Similarly, both pioglitazone and rosiglitazone did not change the contraction induced by U-46619 in rat mesenteric arteries (Mendizábal et al. 2011).
The vasorelaxant effect of PPARγ agonists
Cumulative application of pioglitazone and rosiglitazone caused a concentration-dependent and full relaxation of the endothelium-intact hPAs preconstricted with U-46619. Rosiglitazone proved to be more potent than pioglitazone and the same rank order of potency was also noticed in binding studies to human PPARγ (Fujimura et al. 2006). So, we preferred rosiglitazone as reference PPAR agonist in all further experiments. Importantly, the clinically effective pioglitazone and rosiglitazone blood concentrations of about 0.83–1.82 (Omae et al. 2011) and 0.6–1 μM (Irat et al. 2006), respectively, are contained in the concentration range studied on hPAs in the present investigation. Unlike in hPAs, the maximal vasodilatory effect of rosiglitazone in isolated animal arteries was less than 100 %, namely 45, 40, and 60 % in the mouse pulmonary artery, aorta, and carotid artery, respectively (Ryan et al. 2004; Harrington et al. 2010), 30 % in the rat aorta (Nomura et al. 2008) and 50 % in the porcine retinal artery (Omae et al. 2011). As opposed to the vessels mentioned above, rosiglitazone caused vasoconstriction in human small arteries isolated from subcutaneous fat (Walker et al. 1998).
Rosiglitazone produced a slowly (over 120 min) rather than an acutely developing relaxation of the rat aorta preconstricted with methoxamine (Cunnane et al. 2004) or U-46619 (O’Sullivan et al. 2005). Thus, in additional experiments, we registered the vasodilatory influence of single concentrations of rosiglitazone given separately over 2 h. Again, the PPARγ agonist produced a concentration- and time-dependent, slowly developing decrease in tone of the isolated endothelium-intact hPAs preconstricted with U-46619. Interestingly, the CRCs for rosiglitazone given separately and cumulatively were very similar, and in both cases, full relaxation was noticed. It was induced by 100 μM and was reached after 120 min (administration of a single concentration) and 110 min of incubation (cumulative CRC). The time–effect curve for rosiglitazone 10 μM on the hPA is very similar to that in the rat aorta preconstricted also with U-46619 (O’Sullivan et al. 2005). Thus, in both cases, the first vasodilatory response (by about 15–20 %) occurred after 15 min and maximal relaxation by about 70 % after 120 min.
Mechanisms involved in the rosiglitazone-induced relaxation
Does the vasorelaxant effect of rosiglitazone involve PPARγ receptors? In order to finally examine this point, we examined the influence of GW9662, a potent and selective antagonist of these receptors (Michalik et al. 2006). As a matter of fact, GW9662 1 and 10 μM diminished the rosiglitazone (10 μM)-induced relaxation in hPA after 120 min of incubation by about 35 and 80 %, respectively. In good agreement with our own data, GW9662 1 μM attenuated the rosiglitazone (10 μM)-induced vasorelaxation of the isolated rat aorta after 120 min by about 40 % (O’Sullivan et al. 2005). According to O’Sullivan et al. (2005, 2006), the slow relaxation induced by rosiglitazone is related to the fact that the activation of intracellular PPARγ receptors leads to the transcription of responsive genes.
In further experiments, we demonstrated that endothelium removal reduced the vasorelaxant effect of rosiglitazone in the hPA by about 50 %. Thus, the vasodilatory action of rosiglitazone consists of an endothelium-dependent and endothelium-independent component. Similarly, removal of the endothelium counteracted the vasodilatory effect of rosiglitazone in the rat aorta (Cunnane et al. 2004). Rosiglitazone has also been shown to increase the endothelium-dependent flow in the brachial artery of a healthy man after 6 h (Walcher et al. 2010). Since we were interested in the endothelium-dependent vasodilatory component of rosiglitazone, all further experiments were performed in endothelium-intact vessels.
First, we have checked whether the effect of rosiglitazone might be related to nitric oxide, one of the main endothelial vasodilators. L-NAME, an inhibitor of the biosynthesis of nitric oxide by endothelial cells, attenuated the vasodilatory effect of rosiglitazone, suggesting that nitric oxide plays a role in its effect. Similarly, L-NAME diminished the rosiglitazone-induced relaxation of the rat aorta (Cunnane et al. 2004). In studies from the literature on cultured endothelial cells, both PPARγ-dependent and PPARγ-independent mechanisms of rosiglitazone have been identified. Thus, the rosiglitazone-induced NO synthesis and/or endothelial nitric oxide synthase (eNOS) stimulation was not modified by GW9662 in human aortic (Boyle et al. 2008) but inhibited in porcine iliac artery (Zhao et al. 2011) and completely abolished in human umbilical vein (Polikandriotis et al. 2005) endothelial cells.
Second, a possible role of cyclooxygenase products in the effect of rosiglitazone had to be taken into account. It has been suggested that a combination of prostacyclin analogues and PPARγ receptor agonists may be effective to counteract abnormal vascular remodeling in PAH (for review, see, e.g., Green et al. 2011) since antiproliferative responses to prostacyclin analogues were potentiated by rosiglitazone in peripheral pulmonary arterial smooth muscle cells from patients suffering from idiopathic PAH (Falcetti et al. 2010). We found that the rosiglitazone-induced vasorelaxation of hPA was attenuated by indomethacin, an inhibitor of COX. Moreover, the selective prostacyclin IP receptor antagonist RO1138452 inhibited the rosiglitazone-evoked vasorelaxation of the hPA and showed the same extent of rightward shift as in the case of the CRC of iloprost. Thus, our data suggest that rosiglitazone may increase the formation of vasorelaxant prostacyclin (or another vasorelaxant product of COX activity).
Third, the insulin sensitizer rosiglitazone has been shown to restore, via ATP-sensitive K+ (KATP) channels, the vasorelaxation of human omental arteries impaired by high glucose (Kinoshita et al. 2006). In addition, it has been recently suggested that opening of KATP channels activates eNOS in order to generate NO and thus regulates vasorelaxation (Grossini et al. 2009). Thus, we checked whether KATP channels are involved in the vasodilatory effect of rosiglitazone. Indeed, the vasodilator effect of rosiglitazone was markedly attenuated by glibenclamide, a selective blocker of ATP-activated K+ channels. However, one should keep in mind that in contrast to our results and those obtained by Kinoshita et al. (2006), rosiglitazone, acting via vascular KATP channels, inhibited the isoprenaline-induced coronary vasodilatation in mice (Yu et al. 2011).
Study limitations
As already mentioned above, rosiglitazone showed slow kinetics in human pulmonary arteries. Therefore, it was difficult to reach a plateau for each agonist concentration when the cumulative technique was applied. Nevertheless, since cumulative concentration–response curves to rosiglitazone were established both in the absence and in the presence of inhibitors, the rightward shifts of the curves reflect the blocking effect of the inhibitors. Moreover, one should keep in mind that our patients did not have any clinical evidence of pulmonary hypertension. Thus, pulmonary vessels in the present study might be more responsive to PPARγ agonists than those from patients with PAH (for literature, see “Introduction”). Thus, the presently reported effects may represent an overestimation of their potential use.
Pulmonary arterial hypertension—a new indication for a “difficult” class of drugs?
Our data demonstrating that pioglitazone and rosiglitazone induce a full relaxation of hPAs lend further support to the suggestion made by others (for literature, see “Introduction”) that PPARγ agonists may become useful adjuncts to current therapies for pulmonary hypertension. Importantly, one should keep in mind that, in addition to vasodilatation, PPARγ agonists have beneficial effects on remodeling of pulmonary blood vessels and lung morphology. Thus, chronic treatment with rosiglitazone and/or pioglitazone prevented and/or reversed pulmonary vascular remodeling, neomuscularization, and/or right ventricular hypertrophy induced by monocrotaline (Matsuda et al. 2005) or hypoxia in rats (Crossno et al. 2007; Kim et al. 2010) and in adult (but not in newborn) mice (Nisbet et al. 2010; Nicola et al. 2011). Rosiglitazone also attenuated the proliferation of human pulmonary artery endothelial cells (Kang et al. 2011) and rat pulmonary artery smooth muscle cells (Li et al. 2010) stimulated by hypoxia or serotonin, respectively. An indirect piece of evidence for the suitability of PPARγ agonists in the treatment of PAH is the fact that targeted deletion of PPARγ, in mice smooth muscle (Hansmann et al. 2007) and endothelial cells (Guignabert et al. 2009), results in muscularization of small distal pulmonary arteries and the development of PAH and that, following cessation of hypoxia, PAH persists longer in mice with endothelial PPARγ deletion (Guignabert et al. 2009).
The use of rosiglitazone and pioglitazone, which are indicated for the treatment of type 2 diabetes mellitus (for review, see Michalik et al. 2006; Ciudin et al. 2012), has been restricted or become questionable due to the occurrence of severe side effects (Palee et al. 2011; Ciudin et al. 2012). It is unclear whether the problems associated with the use of the two thiazolidinediones are class effects or are related to particular properties of the single compounds (Ciudin et al. 2012). A new class of drugs, termed selective PPARγ modulators, which show attenuated cardiovascular side effects and are being developed currently, may become alternative drugs for the treatment of type 2 diabetes (Ciudin et al. 2012) and perhaps also of pulmonary arterial hypertension.
Conclusions
Rosiglitazone and pioglitazone cause a full relaxation of the isolated human pulmonary artery. The rosiglitazone-induced effect occurs with a delay, involves PPARγ receptors, and is partially dependent on vascular endothelium. Moreover, it results from (1) the stimulation of NO release from endothelial cells, (2) the activation of IP receptors through production of prostacyclin, and (3) the stimulation of vasodilatory ATP-sensitive K+ channels. Thus, the ability of these thiazolidinediones to relax hPAs is a further piece of evidence that PPARγ agonism may represent a new strategy for the treatment of pulmonary hypertension.
References
Ameshima S, Golpon H, Cool CD, Chan D, Vandivier RW, Gardai SJ, Wick M, Nemenoff RA, Geraci MW, Voelkel NF (2003) Peroxisome proliferator-activated receptor gamma (PPARgamma) expression is decreased in pulmonary hypertension and affects endothelial cell growth. Circ Res 92:1162–1169
Archer SL, Weir EK, Wilkins MR (2010) Basic science of pulmonary arterial hypertension for clinicians: new concepts and experimental therapies. Circulation 121:2045–2066
Boyle JG, Logan PJ, Ewart MA, Reihill JA, Ritchie SA, Connell JM, Cleland SJ, Salt IP (2008) Rosiglitazone stimulates nitric oxide synthesis in human aortic endothelial cells via AMP-activated protein kinase. J Biol Chem 283:11210–11217
Ciudin A, Hernandez C, Simό R (2012) Update on cardiovascular safety of PPARγ agonists and relevance to medicinal chemistry and clinical pharmacology. Curr Top Med Chem 12:585–604
Crossno JT Jr, Garat CV, Reusch JE, Morris KG, Dempsey EC, McMurtry IF, Stenmark KR, Klemm DJ (2007) Rosiglitazone attenuates hypoxia-induced pulmonary arterial remodeling. Am J Physiol Lung Cell Mol Physiol 292:L885–L897
Cunnane SE, Chan YY, Randall MD (2004) Rosiglitazone-induced vasorelaxation in the rat aorta. Proceedings of the British Pharmacological Society at http://www.pa2online.org/Vol2Issue2abst096P.html
Falcetti E, Hall SM, Phillips PG, Patel J, Morrell NW, Haworth SG, Clapp LH (2010) Smooth muscle proliferation and role of the prostacyclin (IP) receptor in idiopathic pulmonary arterial hypertension. Am J Respir Crit Care Med 182:1161–1170
Fujimura T, Sakuma H, Ohkubo-Suzuki A, Aramori I, Mutoh S (2006) Unique properties of coactivator recruitment caused by differential binding of FK614, an anti-diabetic agent, to peroxisome proliferator-activated receptor γ. Biol Pharm Bull 29:423–429
Gong K, Xing D, Li P, Aksut B, Ambalavanan N, Yang Q, Nozell SE, Oparil S, Chen YF (2011) Hypoxia induces downregulation of PPAR-γ in isolated pulmonary arterial smooth muscle cells and in rat lung via transforming growth factor-β signaling. Am J Physiol Lung Cell Mol Physiol 301:L899–907
Green DE, Sutliff RL, Hart CM (2011) Is peroxisome proliferator-activated receptor gamma (PPARγ) a therapeutic target for the treatment of pulmonary hypertension? Pulm Circ 1:33–47
Grossini E, Molinari C, Caimmi PP, Uberti F, Vacca G (2009) Levosimendan induces NO production through p38 MAPK, ERK and Akt in porcine coronary endothelial cells: role for mitochondrial K(ATP) channel. Br J Pharmacol 156:250–261
Guignabert C, Alvira CM, Alastalo TP, Sawada H, Hansmann G, Zhao M, Wang L, El-Bizri N, Rabinovitch M (2009) Tie2-mediated loss of peroxisome proliferator-activated receptor-gamma in mice causes PDGF receptor-beta-dependent pulmonary arterial muscularization. Am J Physiol Lung Cell Mol Physiol 297:L1082–1090
Guimarães S, Moura D (2001) Vascular adrenoceptors: an update. Pharmacol Rev 53:319–356
Hansmann G, Wagner RA, Schellong S, Perez VA, Urashima T, Wang L, Sheikh AY, Suen RS, Stewart DJ, Rabinovitch M (2007) Pulmonary arterial hypertension is linked to insulin resistance and reversed by peroxisome proliferator-activated receptor-gamma activation. Circulation 115:1275–1284
Harrington LS, Moreno L, Reed A, Wort SJ, Desvergne B, Garland C, Zhao L, Mitchell JA (2010) The PPARβ/δ agonist GW0742 relaxes pulmonary vessels and limits right heart hypertrophy in rats with hypoxia-induced pulmonary hypertension. PLoS One 5:e9526
Irat AM, Aslamaci S, Karasu C, Ari N (2006) Alteration of vascular reactivity in diabetic human mammary artery and the effects of thiazolidinediones. J Pharm Pharmacol 58:1647–1653
Jones RL, Wise H, Clark R, Whiting RL, Bley KR (2006) Investigation of the prostacyclin (IP) receptor antagonist RO1138452 on isolated blood vessel and platelet preparations. Br J Pharmacol 149:110–120
Kang BY, Kleinhenz JM, Murphy TC, Hart CM (2011) The PPARγ ligand rosiglitazone attenuates hypoxia-induced endothelin signaling in vitro and in vivo. Am J Physiol Lung Cell Mol Physiol 301:L881–L891
Kim EK, Lee JH, Oh YM, Lee YS, Lee SD (2010) Rosiglitazone attenuates hypoxia-induced pulmonary arterial hypertension in rats. Respirology 15:659–668
Kinoshita H, Azma T, Iranami H, Nakahata K, Kimoto Y, Dojo M, Yuge O, Hatano Y (2006) Synthetic peroxisome proliferator-activated receptor-γ agonists restore impaired vasorelaxation via ATP-sensitive K+ channels by high glucose. J Pharmacol Exp Ther 318:312–318
Kozłowska H, Baranowska M, Schlicker E, Kozłowski M, Laudański J, Malinowska B (2007) Identification of the vasodilatory endothelial cannabinoid receptor in the human pulmonary artery. J Hypertens 25:2240–2248
Li M, Li Z, Sun X, Yang L, Fang P, Liu Y, Li W, Xu J, Lu J, Xie M, Zhang D (2010) Heme oxygenase-1/p21WAF1 mediates peroxisome proliferator-activated receptor-γ signaling inhibition of proliferation of rat pulmonary artery smooth muscle cells. FEBS J 277:1543–1550
Lu X, Murphy TC, Nanes MS, Hart CM (2010) PPARγ regulates hypoxia-induced Nox4 expression in human pulmonary artery smooth muscle cells through NF-κB. Am J Physiol Lung Cell Mol Physiol 299:L559–L566
Matsuda Y, Hoshikawa Y, Ameshima S, Suzuki S, Okada Y, Tabata T, Sugawara T, Matsumara Y, Kondo T (2005) Effects of peroxisome proliferator-activated receptor gamma ligands on monocrotaline-induced pulmonary hypertension in rats. Nihon Kokyuki Gakkai Zasshi 43:283–288
Mendizábal Y, Llorens S, Nava E (2011) Effects of pioglitazone and rosiglitazone on vascular function of mesenteric resistance arteries in rat genetic hypertension. Pharmacology 88:72–81
Michalik L, Auwerx J, Berger JP, Chatterjee VK, Glass CK, Gonzalez FJ, Grimaldi PA, Kadowaki T, Lazar MA, O’Rahilly S, Palmer CN, Plutzky J, Reddy JK, Spiegelman BM, Staels B, Wahlo W (2006) International Union of Pharmacology. LXI. Peroxisome proliferator-activated receptors. Pharmacol Rev 58:726–741
Nicola T, Ambalavanan N, Zhang W, James ML, Rehan V, Halloran B, Olave N, Bulger A, Oparil S, Chen YF (2011) Hypoxia-induced inhibition of lung development is attenuated by the peroxisome proliferator-activated receptor-γ agonist rosiglitazone. Am J Physiol Lung Cell Mol Physiol 301:L125–L134
Nisbet RE, Bland JM, Kleinhenz DJ, Mitchell PO, Walp ER, Sutliff RL, Hart CM (2010) Rosiglitazone attenuates chronic hypoxia-induced pulmonary hypertension in a mouse model. Am J Respir Cell Mol Biol 42:482–490
Nomura H, Yamawaki H, Mukohda M, Okada M, Hara Y (2008) Mechanisms underlying pioglitazone-mediated relaxation in isolated blood vessel. J Pharmacol Sci 108:258–265
Oishi PE, Sharma S, Datar SA, Kumar S, Aggarwal S, Lu Q, Raff G, Azakie A, Hsu JH, Sajti E, Fratz S, Black SM, Fineman JR (2013) Rosiglitazone preserves pulmonary vascular function in lambs with increased pulmonary blood flow. Pediatr Res 73:54–61
Omae T, Nagaoka T, Tanano I, Yoshida A (2011) Pioglitazone, a peroxisome proliferator-activated receptor-γ agonist, induces dilation of isolated porcine retinal arterioles: role of nitric oxide and potassium channels. Invest Ophthalmol Vis Sci 52:6749–6756
O’Sullivan SE, Tarling EJ, Bennett AJ, Kendall DA, Randall MD (2005) Novel time-dependent vascular actions of Delta9-tetrahydrocannabinol mediated by peroxisome proliferator-activated receptor gamma. Biochem Biophys Res Commun 337:824–831
O’Sullivan SE, Kendall DA, Randall MD (2006) Further characterization of the time-dependent vascular effects of Δ9-tetrahydrocannabinol. J Pharmacol Exp Ther 317:428–438
Palee S, Chattipakorn S, Phrommintikul A, Chattipakorn N (2011) PPARγ activator, rosiglitazone: is it beneficial or harmful to the cardiovascular system? World J Cardiol 3:144–152
Polikandriotis JA, Mazzella LJ, Rupnow HL, Hart CM (2005) Peroxisome proliferator-activated receptor γ ligands stimulate endothelial nitric oxide production through distinct peroxisome proliferator-activated receptor γ-dependent mechanisms. Arterioscler Thromb Vasc Biol 25:1810–1816
Ryan MJ, Didion SP, Mathur S, Faraci FM, Sigmund CD (2004) PPARγ agonist rosiglitazone improves vascular function and lowers blood pressure in hypertensive transgenic mice. Hypertension 43:661–666
Salomone S, Drago F (2012) Effects of PPARγ ligands on vascular tone. Curr Mol Pharmacol 5:282–291
Sigmund CD (2010) Endothelial and vascular muscle PPARγ in arterial pressure regulation: lessons from genetic interference and deficiency. Hypertension 55:437–444
Sutliff RL, Kang BY, Hart CM (2010) PPARγ as a potential therapeutic target in pulmonary hypertension. Ther Adv Respir Dis 4:143–160
Walcher T, Walcher D, Hetzel J, Mielke C, Rau M, Rittig K, Balletshofer B, Schwedhelm E, Hombach V, Böger RH, Koenig W, Marx N (2010) Rapid effect of single-dose rosiglitazone treatment on endothelial function in healthy men with normal glucose tolerance: data from a randomised, placebo-controlled, double-blind study. Diab Vasc Dis Res 7:178–185
Walker AB, Naderali EK, Chattington PD, Buckingham RE, Williams G (1998) Differential vasoactive effects of the insulin sensitizers rosiglitazone (BRL 49653) and troglitazone on human small arteries in vitro. Diabetes 47:810–814
Yu L, Jin X, Yang Y, Cui N, Jiang C (2011) Rosiglitazone inhibits vascular KATP channels and coronary vasodilation produced by isoprenaline. Br J Pharmacol 164:2064–2072
Yuen CY, Wong WT, Tian XY, Wong SL, Lau CW, Yu J, Tomlinson B, Yao X, Huang Y (2011) Telmisartan inhibits vasoconstriction via PPARγ-dependent. Cardiovasc Res 90:122–129
Zhao Z, Luo Z, Wang P, Sun J, Yu H, Cao T, Ni Y, Chen J, Yan Z, Liu D, Zhu Z (2011) Rosiglitazone restores endothelial dysfunction in a rat model of metabolic syndrome through PPARγ- and PPARδ-dependent phosphorylation of Akt and eNOS. PPAR Res 2011:291656
Acknowledgments
This work was supported by grants from the Medical University of Białystok (3-13578 F; 113-13613 F).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Kozłowska, H., Baranowska-Kuczko, M., Schlicker, E. et al. Relaxation of human pulmonary arteries by PPARγ agonists. Naunyn-Schmiedeberg's Arch Pharmacol 386, 445–453 (2013). https://doi.org/10.1007/s00210-013-0846-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-013-0846-3