Abstract
Purpose
Perfusion in healthy adults is gravity-dependent. Little is known about lung perfusion in the preterm infant. The aim of this study was to describe the regional distribution of blood volume within the thorax in preterm infants receiving synchronised volume-targeted mechanical ventilation (SIPPV + TTV) and to compare this to regional distribution of tidal ventilation using electrical impedance tomography (EIT).
Methods
Stable supine ventilated preterm infants (<32-week gestation) were studied. Three sets of artefact-free 30-s EIT recordings of the right hemithorax were filtered in the cardiac and respiratory frequency domains to differentiate impedance change due to blood (ΔZ c) and gas volume (ΔZ v). The distribution of ΔZ c and ΔZ v in the anterior-to-posterior regions of the right chest were compared. Infants were subdivided by age (≤7, >7 days) and oxygen requirement.
Results
A total of 5,471 beats were analysed from 26 infants (78 recordings); mean (standard deviation (SD)) gestational age was 26 (2) weeks and mean (SD) postnatal age was 9 (10) days. The median (interquartile range) ΔZ c in the anterior half of the hemithorax was 1.41-fold (0.88–2.11) greater than that in the posterior half. The geometric centre of ΔZ c was located at 46.7% of the anterior-posterior thoracic distance, compared to a more centrally located ΔZ v (49.6%; p < 0.0001). The ΔZ v/ΔZ c ratio was 1.7 in the anterior third of the chest and 2.2 in the posterior (p < 0.0001). The area under the curve (AUC) analysis showed that ΔZ c was more evenly distributed in infants >7 days of age and not influenced by oxygen requirement.
Conclusions
There are gravity dependent differences in the distribution of blood volume and ventilation in the ventilated preterm chest.
Similar content being viewed by others
Introduction
Attempts to improve neonatal ventilation have focused on optimising tidal ventilation and minimising ventilator-induced lung injury [1], but gas exchange is also dependent on lung perfusion [2, 3]. Little is known about lung perfusion and the distribution of blood volume within the preterm lung. The diseased adult lung is particularly prone to ventilation-perfusion mismatching, even when ventilation has been optimised [2]. Understanding lung perfusion and its relationship to ventilation may aid in the respiratory management of preterm infants.
Ventilation and perfusion in adults are not evenly distributed. In healthy upright adults, both ventilation and perfusion have a zonal gravity-dependent distribution from the apex to the base [4]. Regional ventilation-perfusion mismatching is greater in the diseased ventilated adult lung, with over-inflation and under-perfusion predominating in the non-dependent lung regions while the better perfused dependent regions are prone to collapse [2, 5, 6]. In older infants and children, ventilation is preferentially distributed towards the non-dependent lung regardless of disease, which is the reverse of that seen in the healthy adult [7–9], but lung perfusion shows the same gravity-dependent distribution as adults. The result is a reduced ventilation-perfusion ratio in the dependent lung in older infants and children [10]. Whether these differences are present in ventilated preterm infants is unknown.
Traditional methods of determining lung perfusion, such as radio-nuclide scans, are not feasible in the ventilated neonate [10–12]. Electrical impedance tomography (EIT) is a non-invasive, real-time, radiation-free method of measuring the relative change in impedances within regions of a cross-section of the thorax [13–16] that has been validated in newborn infants [19, 20]. Thoracic electrical impedance is influenced by changes in gas, tissue and blood volumes. Air generates a greater impedance change than blood, and EIT has been used to measure regional ventilation in newborn infants [14, 15, 21–25]. Recent technological advances now enable isolation of the EIT signal within the cardiac frequency domain [14, 16, 27], thus potentially allowing determination of cyclical changes in blood volume [12, 26–31]. To date, the distribution of perfusion within the lung of ventilated preterm infants has not been described.
The aim of this study was to describe the relative regional distribution in blood volume within the thorax, using EIT, in preterm infants receiving synchronised, volume-targeted intermittent positive pressure ventilation (SIPPV + TTV) and to compare this to the regional distribution of tidal ventilation.
Methods
Study population
This study was performed in the neonatal intensive care unit (NICU) of The Royal Women’s Hospital, Melbourne from August 2008 to August 2009. The study was approved by the institution’s Human Research Ethics Committee, and informed parental consent was obtained.
Stable infants less than 32 completed weeks’ gestational age at birth and older than 24 h who were receiving SIPPV + TTV via a BabyLog 8000 ventilator (Dräger, Lübeck, Germany) were eligible. The clinical team chose the ventilator settings. Infants were excluded if they were too unstable for routine handling or had an air leak, evolving abdominal pathology, congenital heart disease, a known chromosomal anomaly, refractory hypotension, or an inspired oxygen concentration (F IO2) of >0.9.
Measurements
Oxygen saturation (SpO2), heart rate (HR) and respiratory rate were continuously recorded (IntelliVue MP80 Monitor; Philips, Eindhoven, the Netherlands) and saved at 12-s intervals. Change in thoracic impedance (ΔZ) was measured at nipple level using a GoeMF II EIT system [13, 22] (CareFusion, Hoechberg, Germany) sampling at 44 Hz. To prevent electrode-to-electrode contact, the EIT skin electrodes (Kendall Puppydog 1042PTS; Tyco Healthcare, Mansfield, MA) were pre-trimmed to fit the infant’s chest. Electrodes were placed during routine nursing handling. Prior to any data recording, the quality of electrode conductance and signal stability were verified using the EIT proprietary software (SciEIT; CareFusion) [13]. Inspiratory pressure was measured by the Dräger ventilator at the proximal endotracheal tube, and the analogue signal recorded directly into the EIT unit.
Study methods
At least 30 min after applying the electrodes and while the infant was settled in a supine position, three EIT recordings of 2-min duration were taken approximately 3 min apart. This was repeated 20 min later or when the infant was next settled. During each EIT. the infant’s chest was videoed to aid identification of any movement artefact.
Data collection and analysis
The unfiltered global EIT and pressure data from each 2-min recording were reviewed off-line. To standardise the analysis, from each set of six recordings we selected the last three with at least 30-s of continuously stable, artefact-free, signal and impedance and pressure data extracted.
High- and low-pass filters were applied to the EIT signal at five cycles per minute above and below the highest and lowest recorded HR in order to differentiate the contribution of ΔZ due to blood volume within the chest. Within this frequency domain, the ΔZ is likely to be due to relative changes in blood volume [14, 27]. The ΔZ due to ventilation was determined by applying a low-pass filter at ten cycles per minute above the respiratory rate. Within each frequency domain, the peaks and troughs were identified for each tidal inflation/beat, and the amplitude of impedance change [expressed in countless units (c.u.)] related to heart beat [cardiac frequency domain (ΔZ c)] and ventilation [respiratory frequency domain (ΔZ v)] were determined. The recording was excluded if the HR coincided with a harmonic of the respiratory signal (Fig. 1).
Representative unfiltered and filtered functional electrical impedance tomography (fEIT) images from an infant. a Unfiltered relative impedance change (ΔZ) over 20 s illustrating the difference in ΔZ synchronous with the slower respiratory (peaks marked by solid horizontal line) and faster heart rate (HR; peaks marked by horizontal dashed line). b Frequency content of unfiltered signal. X-axis Frequency (cycles per minute), Y-axis relative weighting of frequency. Solid red lines (0 and 65 cycles per minute) Filtered respiratory domain [respiratory rate 55 beats per minute (BPM)], dashed red lines (175 and 185 cycles per minute) filtered cardiac domain (HR 180 BPM). Arrows indicate harmonics of the respiratory signal. c fEIT image [standard deviation (SD) of ΔZ] of the unfiltered EIT signal. Colour indicates range of relative impedance change (dark blue ΔZ minimum, red ΔZ maximum). d fEIT image of the EIT signal filtered to respiratory domain, demonstrating ventilation within the right and left chest corresponding with the lungs. e fEIT image of the EIT signal filtered to the cardiac domain, demonstrating impedance change in the chest corresponding with the location of the heart (upper centre) and lungs. Each fEIT image is individually scaled to use the entire colour range
A functional EIT (fEIT) image was generated from each recording using the standard deviation (SD) of the impedance time course of each individual pixel within the 32 (anterior to posterior) × 32 (left to right) matrix for ΔZ c and ΔZ v [14, 32, 33]. To minimise the possible effect of the heart and major blood vessels, we analysed ΔZ only in the 32 × 16 pixels encompassing the right hemithorax [34]. For the purpose of determining relative gravity-dependent distribution of ΔZ c and ΔZ v, the values for each parameter in the 16 fEIT pixels within each of the 32 anterior-to-posterior rows of the right hemithorax were summated [23, 25]. The magnitude of ΔZ v and ΔZ c within the anterior and posterior halves of the right hemithorax were compared using area under the curve (AUC) analysis [23, 25]. The anterior-to-posterior geometric centres of ΔZ v and ΔZ c within the right hemithorax were also calculated [13, 25]. To determine the relative regional relationship between the respiratory and cardiac signals, we calculated the ΔZ v/ΔZ c ratio for each pixel. The pooled ΔZ v/ΔZ c ratios within each third of the right hemithorax were compared to aid interpretation. The frequency distribution of all ΔZ v/ΔZ c ratios within each region was also calculated.
As no previous data were available to determine a sample size, a convenience sample of 30 infants was recruited. As both postnatal growth and respiratory disease may influence regional lung development, we performed a sub-group analysis based on age (≤7 vs. >7 days) and respiratory illness severity (air vs. supplemental oxygen). Statistical analysis was performed using GraphPad Prism ver. 4.02 for Windows (Graphpad software, San Diego, CA), and a p value of <0.05 was considered to be significant.
Results
Infant demographics
During the study period there were 63 eligible infants, of whom 30 were recruited. No data were obtained on four infants due to faulty equipment (2 infants), infant death prior to study enrollment (1 infant), and incomplete data (1 infant). We evaluated 78 EIT recordings from 26 infants with a mean (SD) gestational age of 26 (2) weeks. Sixteen infants were studied at ≤7 days and 14 required supplementary oxygen.
All infants were stable on the day of study. The mean (SD) age was 9 (10) days; weight, 889 (309) g; F IO2, 0.27 (0.10); positive end-expiratory pressure (PEEP), 5.6 (0.8) cm H2O; targeted tidal volume (TTV), 4.0 (0.6) mL/kg; HR, 154 (13) BPM. The HR in infants >7 days of age was statistically—but not clinically—significantly greater than that in those ≤7 days, with a mean difference of 10.3 [95% confidence interval (95% CI) 8.6–12.0] BPM (t test). A detailed description of the study population is available in the Electronic Supplemental Material (ESM Table1). Eight infants had or were receiving indomethacin for patent ductus arteriosus (PDA).
Impedance change within cardiac frequency domain
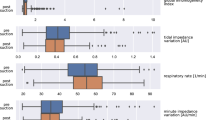
In total, data from 5,520 beats in the right anterior chest and 5,422 beats in the right posterior chest were analysed. Some beats were not suitable for analysis in one region. ΔZ c was greater in the anterior (non-dependent) hemithorax than in the posterior (dependent) hemithorax (also see ESM Table 2). The median ΔZ c in the anterior region was 1.41-fold [interquartile range (IQR) 0.88–2.11] greater than the paired ΔZ c in the posterior region. This difference was more apparent in infants >7 days of age, with an anterior-to-posterior ΔZ c ratio of 1.62 (IQR 0.98–2.33), and in those needing supplemental oxygen (median 1.59, IQR 0.98–2.47) compared to infants ≤7 days in age, with an anterior-to-posterior ΔZ c ratio of 1.29 (IQR 0.82–1.92), and those needing air (median 1.24, IQR 0.81–1.78); both sub-group differences were p < 0.0001 (Mann–Whitney test).
Regional distribution of ΔZ c and ΔZ v
Figure 2a shows fEIT data for ΔZ c and ΔZ v. There was a significant difference in the distribution of ΔZ c and ΔZ v. While ΔZ c was greater in the anterior half of the chest than in the posterior (p < 0.0002, Wilcoxon signed rank test; Table 1), there was no such difference in ΔZ v (p = 0.607). The geometric centre of ΔZ c was located in the anterior (non-dependent) hemithorax, at a mean (SD) of 46.7 (5.0)% of the anterior-to-posterior thoracic distance. The geometric centre of ΔZ c was a mean of 2.9% (95% CI 1.9–3.8) (paired t test) more anterior than the centrally located ΔZ v [mean 49.6 (3.9)% of the anterior-to-posterior thoracic distance].
a The profiles of the amplitude of impedance change in the cardiac frequency domain (∆Zc; open diamonds) and amplitude of impedance change in the respiratory frequency domain (∆Zv; closed circles) for all 32 anterior-to-posterior slices of the right chest, expressed as distance from the anterior (sternum; 0%) to the posterior (vertebra; 100%) chest wall. The overall magnitude of ∆Zv was greater than that of ∆Zc; median [interquartile range (IQR)] area under the curve (AUC) 21.1 (10.9–28.7) vs. 6.4 (3.9–11.1) c.u., respectively; p < 0.0001 (Wilcoxon signed-rank test). ∆Zc was distributed towards the anterior half of the right chest (p = 0.0002, Wilcoxon signed-rank test) with the mean (SD) geometric centre of ΔZc (dashed line) being located at 46.7 (5.0)% of the anterior-to-posterior thoracic distance. There was no difference in the distribution of ∆Zv within the right chest, which was centrally located at 49.6 (3.9)% (solid line; p < 0.0001, paired t test). b Profile of ∆Zc (diamonds) and ∆Zv (circles) for infants ≤7 days old (open symbols) and >7 days old (closed symbols). Both ∆Zc and ∆Zv increased with age. The distribution of ∆Zc was more anterior in infants ≤7 days old. c Profile of ∆Zc (diamonds) and ∆Zv (circles) for those infants ventilated in air (open symbols) and supplemental oxygen (closed symbols). For both ∆Zc and ∆Zv, the need for supplemental oxygen did not alter the distribution of impedance. All symbols are mean and standard error
ΔZ c and ΔZ v increased with age within all thoracic regions (Fig. 2b). Age ≤7 days resulted in a more anterior distribution of ΔZ c, with the geometric centre of ΔZ c being located at a mean (SD) 45.5 (5.1)% in infants ≤7 days compared to 48.7 (4.1)% in those infants >7 days (mean difference −3.2, 95% CI −5.4 to −1.0). The distribution of ΔZ v was not influenced by age. The mean (SD) geometric centre of ΔZ v was 49.3 (3.7)% and 50.0 (4.1)% for those infants ≤ 7 and >7 days, respectively. The need for supplemental oxygen did not significantly alter the regional distribution of ΔZ c or ΔZ v (Fig. 2c), with the geometric centre of ΔZ c being at 46.9 (3.0) and 46.6 (5.8)% for air and oxygen, respectively, compared to 49.0 (3.5) and 50.1 (4.1)% for ΔZ v.
ΔZ v/ΔZ c ratio
The closest ΔZ v to ΔZ c matching occurred in the anterior right hemithorax. Within this region, the median (25–75% IQR) ΔZ v/ΔZ c ratio was 1.7 (1.3–2.2) compared to 1.8 (1.4–2.3) and 2.2 (1.7–2.9) in the middle and posterior thirds (p < 0.0001, Kruskal–Wallis test).
Figure 3 shows the regional differences in ΔZ v/ΔZ c ratios by sub-group. In all sub-groups, the ΔZ v/ΔZ c ratio increased with increasing gravity dependency (all p < 0.0001, Kruskal–Wallis test). There was a non-significant trend towards a lower ΔZ v/ΔZ c ratio within the posterior region for those infants in air compared to oxygen. This result may suggest that ventilation-perfusion approaches a more even distribution in this sub-group. ESM Fig. 1 shows the relative frequency of the ΔZ v/ΔZ c ratios within each region.
∆Z v/∆Z c ratio within the anterior (white), middle (grey), and posterior (black) thirds of the right chest for infants ≤7, >7 days old, ventilated in air, and requiring supplementary oxygen. In all sub-groups, the ∆Z v/∆Z c ratio increased with increasing gravity dependency (all p < 0.0001, Kruskal–Wallis test; p < 0.01 †anterior vs. middle and ‡middle vs. posterior thirds, Dunn’s multiple comparison post test). There was a non-significant trend towards a more even distribution in those infants >7 days old and ventilated in air. All data are given as the median and IQR
Discussion
Premature infants with respiratory failure represent a clinical challenge. Understanding the effect of blood flow, and its relationship with tidal ventilation, within the diseased lung may help in optimising oxygenation while minimising the harmful effects of ventilation [3, 35]. The importance of lung perfusion is frequently overlooked There is increasing awareness that the distribution of ventilation within the diseased neonatal lung is inhomogeneous [36]. This is the first study to describe regional blood volume changes within the preterm lung and correlate them with ventilation. Our data suggest that pulsatile changes in impedance within the cardiac domain vary within the newborn chest. Impedance change and, by assumption, change in blood volume, was greater in the non-dependent half of the right hemithorax.
Electrical impedance tomography is a new non-invasive technique that has been validated in neonates, though mainly for studying ventilation [14–20, 24]. Our study demonstrates that describing impedance change within different frequency domains is possible, even in the small neonatal chest. Technological advances that enable the complex EIT signal to be filtered has allowed assessment of impedance change due to pulmonary blood flow in adults and animal models [12, 26–30]. Compared to the adult, when the HR is closer to respiratory rate, delineation of the harmonics of the respiratory and cardiac frequencies may be simpler in the neonate.
The effect of cardiac structures on the impedance signal is uncertain [26]. It is possible that impedance changes within the cardiac domain are due to transmitted waveforms or impulses from the heart and major blood vessels, and not to blood volume change within the lung itself. Despite limiting our analysis to the right hemithorax, this possibility may explain our finding of an increased frequency of ΔZ v/ΔZ c ratios <1.0 within the anterior third of the chest, although it does not account for the majority of ΔZ v/ΔZ c ratios being >1.0. In adults, impedance changes measured by EIT within the cardiac domain do represent reproducible fluctuations in perfusion within the lung rather than changes in cardiac output [26, 28]. Smit and co-workers [28] identified that impedance change filtered to the cardiac domain was affected by the size of the pulmonary microvascular bed rather than by stroke volume or changes in cardiac output. Regional perfusion measured by EIT correlates well with computed tomography imaging and radio-nuclide scanning [37, 38].
Some infants had a PDA considered to be significant by the clinicians. As echocardiography was not part of the study and some of the infants with a PDA were undergoing treatment, conclusions about the potential effect of a PDA on ∆Z c cannot be made. More detailed studies in this area are indicated.
In our study, the ∆Z c was increased in the non-dependent region of the chest and less centrally distributed than ventilation. The traditional view that perfusion is distributed towards gravity-dependant regions of the lung [4] has recently been disputed [39, 40]. Regional differences in lung perfusion are variable and may be influenced by heterogeneity of the pulmonary vascular anatomy, regional variations in vascular tone and resistance and hydrostatic pressure differences within the chest [39, 40]. These causes would better explain the more even distribution of perfusion noted in adults after prone positioning [5, 6, 34].
The relative regional distribution of blood volume and tidal ventilation differed in the infants studied. Compared to ΔZ v, the anterior-to-posterior distribution of ΔZ c was more variable. This difference was expressed in the frequency distribution of the ΔZ v/ΔZ c ratios. In the posterior region, there was an overall increase in the ΔZ v/ΔZ c ratio compared to the other regions, implying an increase in areas of ventilation-perfusion mismatching. As one might expect, there was a trend to a more even distribution of the ΔZ v/ΔZ c ratio in those infants not requiring supplemental oxygen, suggesting improved ventilation-perfusion matching. Regional differences in perfusion have been similarly documented in adults with lung disease [6]. In this population, the gravity-dependent variation in ventilation-perfusion is reduced with turning from supine to prone [5, 6, 34]. Clinically prone positioning is used to improve ventilation-perfusion matching and oxygenation while avoiding potentially harmful increases in applied positive pressure during acute respiratory failure in adults [3, 5, 6]. Ventilated preterm infants are frequently nursed in different positions. Investigating the influence of position on the distribution of ventilation and blood flow in premature infants is therefore warranted.
The ΔZ c among our patients became more evenly distributed with increasing postnatal age, with a resultant reduction in the difference between the geometric centres and regional magnitudes of ΔZ c and ΔZ v. In animal models of the healthy neonatal lung, postnatal growth results in a temporary adaption in perfusion towards the non-dependent (dorsal) region of the lung [39]. Ventilation strategies that aggressively recruit the dependent lung to maximise gas exchange [36] therefore may be less effective in early neonatal life.
Caution should be exercised when extrapolating our understanding of the healthy adult lung to the preterm. The diseased ventilated preterm lung, chest wall and circulatory system differ from those of the healthy, non-ventilated newborn, child or adult. For this reason, our findings were not compared to a non-ventilated neonatal population. The infants in this study were stable and recovering from the acute phase of surfactant-deficiency, explaining the evenly distributed ΔZ v. This study could aid future studies of premature infants with severe respiratory failure in whom the interaction between ventilation and lung perfusion is likely to be of greater importance.
Our study has a number of limitations. Calibration of the impedance signals to a known parameter is not possible, limiting the EIT to an assessment of relative changes. Consequently, caution should be exercised in the interpretation of raw impedance values between subjects. Normalisation to a global parameter does not necessarily overcome this limitation. However, the reproducibility of the distribution of the beat-to-beat and ΔZ c data within our population is reassuring and suggests that the EIT may have a role in assessing changes within a patient over time. Generating fEIT images from the standard deviation of the impedance time course is common practice and allows researchers to compare the regional distribution of ΔZ between subjects [16]. This technique, which quantifies the relative magnitude, but not the direction, of impedance change, may be misleading to inexperienced operators [41]. Lead placement was difficult in the extremely preterm newborn due to the small chest circumference. The potential for electrode contact and subsequent artefact is high, even when the leads are trimmed. In addition, small changes in the lead placement may result in relatively large changes in the region of lung examined by the EIT. In adults, the intra-operative reproducibility of EIT has been found to be high [29]. The NICU is an electrically rich environment and the potential for interference high. Despite these limitations, the EIT assessment of thoracic impedance changes was both feasible and well-tolerated. Finally, while this study is the largest of its kind performed to date, the sample size was relatively small, limiting sub-group analysis to arbitrary groups. A larger study of preterm infants involving a diverse range of disease severity and ventilation approaches is justified.
Conclusion
This is the first study to describe the relationship between ventilation and blood volume changes within the mechanically ventilated preterm lung. Regional blood volume changes were greater in the non-dependent lung and influenced by age. These findings suggest that lung perfusion may be distributed towards the non-dependent lung and that it differs from the distribution of ventilation. This study has shown that the EIT is feasible, and well tolerated, in preterm infants.
Abbreviations
- BPM:
-
Beats/breaths per minute
- c.u.:
-
Countless impedance units
- EIT:
-
Electrical impedance tomography
- fEIT:
-
Functional electrical impedance tomography
- F IO2 :
-
Fraction of inspired oxygen concentration
- HR:
-
Heart rate
- PDA:
-
Patent ductus arteriosus
- SIPPV:
-
Synchronised intermittent positive pressure ventilation
- SIPPV + TTV:
-
Synchronised volume-targeted intermittent positive pressure ventilation
- TTV:
-
Targeted tidal volume (volume guarantee)
- ΔZ :
-
Change in thoracic impedance
- ΔZ c :
-
Amplitude of impedance change in the cardiac frequency domain
- ΔZ v :
-
Amplitude of impedance change in the respiratory frequency domain
References
van Kaam AH, Rimensberger PC (2007) Lung-protective ventilation strategies in neonatology: what do we know—what do we need to know? Crit Care Med 35:925–931
Dueck R (2006) Alveolar recruitment versus hyperinflation: a balancing act. Curr Opin Anaesthesiol 19:650–654
Gattinoni L, Carlesso E, Valenza F, Chiumello D, Caspani ML (2004) Acute respiratory distress syndrome, the critical care paradigm: what we learned and what we forgot. Curr Opin Crit Care 10:272–278
West JB (1978) Regional differences in the lung. Chest 74:426–437
Dries DJ (1998) Prone positioning in acute lung injury. J Trauma 45:849–852
Mure M, Lindahl SG (2001) Prone position improves gas exchange—but how? Acta Anaesthesiol Scand 45:150–159
Heaf DP, Helms P, Gordon I, Turner HM (1983) Postural effects on gas exchange in infants. N Engl J Med 308:1505–1508
Davies H, Kitchman R, Gordon I, Helms P (1985) Regional ventilation in infancy. Reversal of adult pattern. N Engl J Med 313:1626–1628
Davies H, Helms P, Gordon I (1992) Effect of posture on regional ventilation in children. Pediatr Pulmonol 12:227–232
Bhuyan U, Peters AM, Gordon I, Davies H, Helms P (1989) Effects of posture on the distribution of pulmonary ventilation and perfusion in children and adults. Thorax 44:480–484
Wolf GK, Arnold JH (2005) Noninvasive assessment of lung volume: respiratory inductance plethysmography and electrical impedance tomography. Crit Care Med 33[Suppl]:S163–S169
Vonk-Noordegraaf A, van Wolferen SA, Marcus JT, Boonstra A, Postmus PE, Peeters JW, Peacock AJ (2005) Noninvasive assessment and monitoring of the pulmonary circulation. Eur Respir J 25:758–766
Frerichs I, Dargaville PA, van GH, Morel DR, Rimensberger PC (2006) Lung volume recruitment after surfactant administration modifies spatial distribution of ventilation. Am J Respir Crit Care Med 174:772–779
Dunlop S, Hough J, Riedel T, Fraser JF, Dunster K, Schibler A (2006) Electrical impedance tomography in extremely prematurely born infants and during high frequency oscillatory ventilation analyzed in the frequency domain. Physiol Meas 27:1151–1165
Pillow JJ, Frerichs I, Stocks J (2006) Lung function tests in neonates and infants with chronic lung disease: global and regional ventilation inhomogeneity. Pediatr Pulmonol 41:105–121
Bodenstein M, David M, Markstaller K (2009) Principles of electrical impedance tomography and its clinical application. Crit Care Med 37:713–724
Brown BH, Primhak RA, Smallwood RH, Milnes P, Narracott AJ, Jackson MJ (2002) Neonatal lungs—can absolute lung resistivity be determined non-invasively? Med Biol Eng Comput 40:388–394
Smallwood RH, Hampshire AR, Brown BH, Primhak RA, Marven S, Nopp P (1999) A comparison of neonatal and adult lung impedances derived from EIT images. Physiol Meas 20:401–413
Marven SS, Hampshire AR, Smallwood RH, Brown BH, Primhak RA (1996) Reproducibility of electrical impedance tomographic spectroscopy (EITS) parametric images of neonatal lungs. Physiol Meas 17[Suppl]:A205–A212
Hampshire AR, Smallwood RH, Brown BH, Primhak RA (1995) Multifrequency and parametric EIT images of neonatal lungs. Physiol Meas 16[Suppl]:A175–A189
Frerichs I, Schiffmann H, Hahn G, Hellige G (2001) Non-invasive radiation-free monitoring of regional lung ventilation in critically ill infants. Intensive Care Med 27:1385–1394
Heinrich S, Schiffmann H, Frerichs A, Klockgether-Radke A, Frerichs I (2006) Body and head position effects on regional lung ventilation in infants: an electrical impedance tomography study. Intensive Care Med 32:1392–1398
Riedel T, Kyburz M, Latzin P, Thamrin C, Frey U (2009) Regional and overall ventilation inhomogeneities in preterm and term-born infants. Intensive Care Med 35:144–151
Frerichs I, Schiffmann H, Oehler R, Dudykevych T, Hahn G, Hinz J, Hellige G (2003) Distribution of lung ventilation in spontaneously breathing neonates lying in different body positions. Intensive Care Med 29:787–794
Schibler A, Yuill M, Parsley C, Pham T, Gilshenan K, Dakin C (2009) Regional ventilation distribution in non-sedated spontaneously breathing newborns and adults is not different. Pediatr Pulmonol 44:851–858
Vonk Noordegraaf A, Kunst PW, Janse A, Marcus JT, Postmus PE, Faes TJ, de Vries PM (1998) Pulmonary perfusion measured by means of electrical impedance tomography. Physiol Meas 19:263–273
Zadehkoochak M, Blott BH, Hames TK, George RF (1992) Pulmonary perfusion and ventricular ejection imaging by frequency domain filtering of EIT (electrical impedance tomography) images. Clin Phys Physiol Meas 13[Suppl]:A191–A196
Smit HJ, Vonk-Noordegraaf A, Marcus JT, Boonstra A, de Vries PM, Postmus PE (2004) Determinants of pulmonary perfusion measured by electrical impedance tomography. Eur J Appl Physiol 92:45–49
Smit HJ, Handoko ML, Vonk-Noordegraaf A, Faes TJ, Postmus PE, de Vries PM, Boonstra A (2003) Electrical impedance tomography to measure pulmonary perfusion: is the reproducibility high enough for clinical practice? Physiol Meas 24:491–499
Smit HJ, Vonk-Noordegraaf A, Marcus JT, van der Weijden S, Postmus PE, de Vries PM, Boonstra A (2003) Pulmonary vascular responses to hypoxia and hyperoxia in healthy volunteers and COPD patients measured by electrical impedance tomography. Chest 123:1803–1809
Frerichs I, Pulletz S, Elke G, Reifferscheid F, Schadler D, Scholz J, Weiler N (2009) Assessment of changes in distribution of lung perfusion by electrical impedance tomography. Respiration 77:282–291
Barber DC (1989) A review of image reconstruction techniques for electrical impedance tomography. Med Phys 16:162–169
Barber DC (1989) A sensitivity method for electrical impedance tomography. Clin Phys Physiol Meas 10:368–371
Nyren S, Mure M, Jacobsson H, Larsson SA, Lindahl SG (1999) Pulmonary perfusion is more uniform in the prone than in the supine position: scintigraphy in healthy humans. J Appl Physiol 86:1135–1141
Polglase GR, Morley CJ, Crossley KJ, Dargaville P, Harding R, Morgan DL, Hooper SB (2005) Positive end-expiratory pressure differentially alters pulmonary hemodynamics and oxygenation in ventilated, very premature lambs. J Appl Physiol 99:1453–1461
Tingay DG, Mills JF, Morley CJ, Pellicano A, Dargaville PA (2006) The deflation limb of the pressure–volume relationship in infants during high-frequency ventilation. Am J Respir Crit Care Med 173:414–420
Frerichs I, Hinz J, Herrmann P, Weisser G, Hahn G, Quintel M, Hellige G (2002) Regional lung perfusion as determined by electrical impedance tomography in comparison with electron beam CT imaging. IEEE Trans Med Imaging 21:646–652
Kunst PW, Vonk NA, Hoekstra OS, Postmus PE, de Vries PM (1998) Ventilation and perfusion imaging by electrical impedance tomography: a comparison with radionuclide scanning. Physiol Meas 19:481–490
Glenny RW, Bernard SL, Luchtel DL, Neradilek B, Polissar NL (2007) The spatial–temporal redistribution of pulmonary blood flow with postnatal growth. J Appl Physiol 102:1281–1288
Galvin I, Drummond GB, Nirmalan M (2007) Distribution of blood flow and ventilation in the lung: gravity is not the only factor. Br J Anaesth 98:420–428
Pulletz S, Elke G, Zick G, Schädler D, Scholz J, Weiler N, Frerichs I (2008) Performance of electrical impedance tomography in detecting regional tidal volumes during one-lung ventilation. Acta Anaesthesiol Scand 52:1131–1139
Acknowledgements
The authors wish to thank Brenda Argus and Stephanie Tan-Kristanto for their assistance with this study. D.G.T. is supported by a National Health and Medical Research Council Clinical Research Fellowship (Grant ID 491286), P.G.D. is supported by a NHMRC Practitioner Fellowship.
Conflict of interest
The authors declare that there are no competing interests.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
134_2010_2049_MOESM2_ESM.pdf
Distribution of all the ΔZv/ΔZc ratios within the anterior (red line), middle (black line) and posterior (blue line) thirds of the right chest from the 78 EIT recordings (PDF 33 kb)
Rights and permissions
About this article
Cite this article
Carlisle, H.R., Armstrong, R.K., Davis, P.G. et al. Regional distribution of blood volume within the preterm infant thorax during synchronised mechanical ventilation. Intensive Care Med 36, 2101–2108 (2010). https://doi.org/10.1007/s00134-010-2049-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-010-2049-4