Abstract
Background
The impact of antibiotic resistance on the outcome of infections due to Gram-negative bacilli, especially Pseudomonas, remains highly controversial.
Study objective, design, and patients
We evaluated the impact of piperacillin resistance on the outcomes of Pseudomonas aeruginosa ventilator-associated pneumonia (VAP) for patients who had received appropriate empiric antibiotics before enrollment in the PNEUMA trial, a multicenter randomized study comparing 8 vs 15 days of antibiotics.
Results
Despite similar characteristics at intensive care unit (ICU) admission, patients infected with piperacillin-resistant Pseudomonas strains were more acutely ill at VAP onset and had a higher 28-day mortality rate (37 vs 19%; P = 0.04) than those with piperacillin-susceptible Pseudomonas VAP. Factors associated with 28-day mortality retained by multivariable analysis were: age (OR: 1.07; 95% CI: 1.03–1.12); female gender (OR: 4.00; 95% CI: 1.41–11.11); severe underlying comorbidities (OR: 2.73; 95% CI: 1.02–7.33); and SOFA score (OR: 1.17; 95% CI: 1.03–1.32), but piperacillin resistance did not reach statistical significance (OR: 2.00; 95% CI: 0.72–5.61). The VAP recurrence rates, either superinfection or relapse, and durations of mechanical ventilation and ICU stay did not differ as a function of Pseudomonas-resistance status.
Conclusions
For patients with Pseudomonas VAP benefiting from appropriate empiric antibiotics, piperacillin resistance was associated with increased disease severity at VAP onset and higher 28-day crude mortality; however, after controlling for confounders, piperacillin-resistance was no longer significantly associated with 28-day mortality. The VAP recurrence rates and durations of ICU stay and mechanical ventilation did not differ for susceptible and resistant strains.
Similar content being viewed by others
Introduction
Ventilator-associated pneumonia (VAP) remains one the most serious complications of mechanical ventilation (MV) and the nosocomial infection with the highest associated mortality [1]. Pseudomonas aeruginosa, one of the bacteria most frequently responsible for VAP, is also one of the most virulent, associated with the worst morbidity and mortality rates [2, 3]. In addition, antibiotic resistance of this bacterium has markedly increased in recent years, reaching rates > 30% for antipseudomonal third-generation cepholosporins or quinolones [4].
It has been hypothesized that infections caused by this highly antibiotic-resistant pathogen might result in higher mortality, longer durations of hospitalization, and greater costs, compared with infections due to antibiotic-susceptible strains [5, 6]; however, to date, conflicting data from a limited number of studies on the impact of antibiotic resistance on the outcomes of severe infections due to Gram-negative bacilli, especially Pseudomonas, have been reported [5, 7, 8, 9, 10, 11, 12, 13, 14]. Furthermore, inappropriate initial empiric antimicrobial treatment, which was among the strongest independent determinants of in-hospital mortality in two recent studies on Pseudomonas bacteremia [10, 12], might represent one of the major confounders in studying the consequences of antibiotic resistance on infection outcomes.
The aim of this study was therefore to evaluate the impact of piperacillin resistance on the outcomes of Pseudomonas VAP for patients who had received appropriate empiric antibiotics for VAP before enrollment in the large cohort of the PNEUMA trial [15].
Patients and methods
The PNEUMA trial [15] was a prospective multicenter, randomized, double-blind (until day 8) clinical trial conducted at 51 intensive care units (ICUs) in France, that demonstrated the equivalence of 8 vs 15 days of antibiotics in terms of clinical outcomes for patients with microbiologically proven VAP. Among the 401 patients enrolled in that trial, 115 had Pseudomonas aeruginosa VAP.
Data collection
At ICU admission, the following data were recorded for each patient: age; gender; severity of underlying medical condition, according to the criteria of McCabe and Jackson [16]; Simplified Acute Physiology Score (SAPS II) [17]; Sepsis-related Organ Failure Assessment (SOFA) score [18]; Organ Dysfunctions and/or INfection (ODIN) score [19]; and the primary reason for initiating MV.
On the day of bronchoscopy (day 1), we recorded the following: duration of prior MV; SAPS II; ODIN and SOFA scores; temperature; leukocyte count; PaO2/FIO2 ratio; radiological score [20]; blood-culture positivity; and presence of shock or acute respiratory distress syndrome [21]. Only piperacillin susceptibility for Pseudomonas aeruginosa was recorded in the PNEUMA database.
Microbiological methods
Pseudomonas aeruginosa was identified by standard microbiological methods. Piperacillin susceptibility was determined using the disk-diffusion test. According to the criteria of the Antibiogram Committee of the French Society for Microbiology, the organism was considered “susceptible” when the inhibition diameter was > 18 mm, “intermediate” (denoting “intermediately susceptibility”) when the diameter was 12–17 mm, and “resistant” when the diameter was < 12 mm, all for a disk content of 75 mg of antimicrobial agent [22]. Intermediate susceptibility to piperacillin was considered to be resistance, because piperacillin was never prescribed for intermediate strains in such cases.
Follow-up
The following data were recorded daily during the 28-day period following the initial bronchoscopy: temperature; leukocyte counts; PaO2/FIO2; presence or absence of purulent tracheal secretions, whether the patient was still mechanically ventilated or not; vital signs, and ODIN score. The SOFA and radiological scores were determined on days 3, 7, 14, 21, and 28. Extreme vigilance for pneumonia recurrence was maintained throughout the study period to detect any possible relapse or new episode of pulmonary infection, and fiberoptic bronchoscopy was performed before the introduction of any new antibiotics as soon as a patient became febrile, had purulent tracheal secretions, and/or a new pulmonary infiltrate developed or an existing infiltrate progressed. Distal pulmonary secretions were also collected bronchoscopically when unexplained hemodynamic instability required higher vasopressor doses (> 30%) or their introduction; in the case of unexplained deterioration of blood gases, with a PaO2/FIO2 decrease of > 30%; or when an intercurrent event imposed an urgent change of antibiotic therapy, regardless of the reason. Any antibiotic use was recorded daily until day 28.
Outcome measures
Death from any cause was recorded until day 60. We recorded the durations of MV and ICU stay after VAP onset. We calculated the number of MV-free days as the number of days during the 28 days after inclusion when the patient was alive and not on MV. Patients were considered to have microbiologically documented recurrent pulmonary infection when at least one bacterial species grew at a significant concentration from samples collected during a second bronchoscopy. Recurrence was considered a relapse if the initial causative bacterial strains (i.e., same genus, species, and serotype when available) grew at a significant concentration from a second distal sample; otherwise, it was considered to be a superinfection.
Statistical analyses
Continuous variables were compared with Student's t-test or the Mann–Whitney U-test, as appropriate. Categorical variables were compared with chi-square tests. To examine the univariate effects of patients' clinical characteristics and initial ICU events on the outcome of interest, a logistic regression model was used to test each characteristic. Thereafter, we undertook multiple logistic regressions using backward stepwise variable elimination (with variable exit threshold set at P > 0.05). Factors with P ≤ 0.10 in our univariable analysis were entered into the model and treatment duration was forced into each of the final models as a covariate [23]. All potential explanatory variables included in the multivariable analyses were subjected to a correlation matrix for analysis of colinearity. Variables with association among each other were not included in the multivariable model. Interactions were explored between the substantive variables that remained in the multivariablemodels. Cumulative-event curves were estimated with the Kaplan-Meier method, and the groups compared using the log-rank test. Statistical significance was defined as p < 0.05. Analyses were performed using StatView 5.0 (SAS Institute Inc., Cary, N.C.) and SPSS 11.5 (SPSS Inc., Chicago, Ill.) software.
Results
Study population
Of the 115 Pseudomonas aeruginosa VAP episodes, 63 (55%) were due to piperacillin-resistant (PRPA) and 52 (45%) to piperacillin-susceptible (PSPA) strains, respectively. At ICU admission (Table 1), no statistically significant difference was detected as a function of Pseudomonas-resistance status, although PRPA-infected patients tended to have more severe premorbid conditions; however, at VAP onset (Table 2), PRPA patients had significantly higher SAPS II, SOFA, and ODIN scores, and had signs of more severe pulmonary lesions, as indicated by their higher radiological scores. Early onset, polymicrobial VAP rates, and physiological parameters did not differ significantly between the two groups. Finally, the percentages of patients included in the 15-day and 8-day treatment groups were similar.
Antibiotic therapy
Every patient included in the PNEUMA trial received, within the 24 h following bronchoscopy, appropriate antibiotic therapy directed against the microorganism(s) responsible for the pulmonary infection, as determined by their susceptibility patterns. During the first week of treatment, every patient received at least two antibiotics active against Pseudomonas: 112 received an anti-pseudomonal β-lactam agent in association with an aminoglycoside (94 cases), a fluoroquinolone (49 cases) or colimycin (8 cases), and three received a fluoroquinolone in association with an aminoglycoside and/or colimycin. The β-lactam agent administered to PRPA-infected patients after microbiological culture results was ceftazidime in 28 cases, piperacillin/tazobactam in 18 cases, imipenem in 10 cases, cefipime in 3 cases, and ticarcillin/clavulanate in 2 cases.
Factors associated with death within 28 days of bronchoscopy
By day 28, 10 (19%) PSPA-infected and 23 (37%) PRPA-infected patients had died (OR = 2.42, 95% CI, 1.02–5.70; P = 0.04; Table 3). Univariable analysis of factors potentially associated with 28-day mortality identified age, female gender, McCabe and Jackson score, day-1 disease-severity and organ-dysfunction scores, shock on day 1 and piperacillin resistance (Table 4). Independent predictors of 28-day mortality retained by multivariable logistic-regression analysis were: age; female gender; McCabe and Jackson score; and day-1 SOFA score; but not piperacillin resistance (OR = 2.00, 95% CI, 0.72–5.61, P = 0.19, when this variable was forced into the final multivariable model).
Other clinical outcomes
As indicated in Table 3, 60-day and in-hospital mortality were significantly higher for PRPA-infected patients. All the other outcomes evaluated—percentages of patients developing VAP recurrence, either relapse or superinfection, or durations of MV, MV-free days, and ICU stay after VAP onset—did not differ significantly between groups.
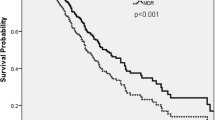
Figure 1 shows the evolution of physiological and functional scores from day 1 to day 28. Temperature, leukocyte count, PaO2/FIO2, and radiological score did not differ significantly between groups, whereas leukocyte count and radiological score tended to be higher for PRPA VAP. Organ-dysfunction scores were higher for PRPA VAP patients, but improved in parallel with those of PSPA episodes, with the significant differences fading at later time points.
Physiological and functional score changes from day 1 (day of bronchoscopy) to day 28. Open circles: patients with piperacillin-resistant Pseudomonas aeruginosa VAP; closed circles: patients with piperacillin-susceptible Pseudomonas aeruginosa ventilator-associated pneumonia (VAP). SOFA Sepsis-related Organ Failure Assessment; ODIN Organ Dysfunction and/or INfection
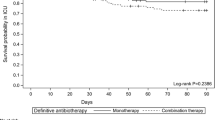
Finally, as shown in Fig. 2, Kaplan-Meier estimates of the cumulative probabilities of survival were not different for the 8-day and 15-day treatment groups, for PSPA- and PRPA-infected patients (log-rank = 0.49 and 0.76, respectively).
Discussion
The aim of this study was to evaluate the impact of piperacillin resistance on the outcome of Pseudomonas VAP on a large cohort of patients who had received appropriate empiric antibiotics. Our main findings were that, despite similar characteristics at ICU admission, patients infected with PRPA strains were more acutely ill at VAP onset and their mortality rate was higher. Factors associated with death 28 days after VAP onset retained by multivariable analysis were age, female gender, severity of underlying comorbidities, and SOFA score, but not piperacillin resistance. Rates of VAP recurrence, either superinfection or relapse, and durations of MV and ICU stay were comparable for the two patient groups.
To date, no published study has specifically addressed the impact of antibiotic resistance on the outcomes of Gram-negative bacilli VAP. In a retrospective cohort study evaluating epidemiological characteristics of 34 PRPA and 101 PSPA VAP episodes, our analysis demonstrated that factors associated with PRPA VAP were underlying fatal medical condition, prior fluoroquinolone use, and less severe disease at ICU admission [14]. In that study, we did not find higher recurrence or death rates for PRPA infections, but we did not control for the appropriateness of empiric antibiotics and patients with PRPA VAP had been less severely ill at ICU admission [14].
Other studies comparing outcomes of susceptible and resistant Gram-negative bacilli infections are scarce. In a case-control study on Gram-negative infections, significant predictors of a fatal outcome were age, APACHE II score, and site of infection, but not antibiotic resistance (23.6 vs 29.2%; P = 0.35) [13]. Furthermore, analysis of all Pseudomonas aeruginosa infections in that population demonstrated no significant difference in mortality between resistant and sensitive strains (18.9 vs 20.0%, P = 0.85) [13]. In a study evaluating health and economic outcomes of resistant Pseudomonas infections, Carmeli et al. [5] found that only the emergence of these resistant strains during the hospital stay was associated with prolonged length of stay and higher in-hospital mortality, while patients with resistant strains at hospital admission did not have a poorer prognosis. In a more recent study by the same group, patients infected with multiresistant Pseudomonas strains had higher mortality rates and longer duration of hospital stays [9], but the control patients in that study did not have Pseudomonas infections. Data from the few studies of Gram-negative bacteremia have also provided similar results. In a case-control study on neutropenic cancer patients, Spanik et al. [24] failed to demonstrate that attributable mortality was higher for antibiotic-resistant Gram-negative bacilli. Similarly, in a retrospective study on antibiotic-susceptible and antibiotic-resistant nosocomial Gram-negative bacillus bacteremia, Blot et al. [7] did not find higher mortality for patients infected with resistant strains. In that study, in-hospital mortality was 57% for antibiotic-resistant and 64% for antibiotic-susceptible Pseudomonas strains. More recently, analyzing data of 190 episodes of Pseudomonas bacteremia, Kang et al. [11] reported that 30-day mortality was comparable for susceptible and resistant strains (34 vs 44%, P = 0.16, respectively).
The higher crude mortality frequently reported for infections caused by antibiotic-resistant organisms could reflect characteristics of the bacterium itself (enhanced virulence for resistant strains), host factors (patient characteristics may differ between groups), or to the antimicrobial treatment administered to patients infected with antibiotic-resistant bacteria [6]. Indeed, inappropriate initial empiric antimicrobial treatment was among the independent factors associated with death according to multivariable analyses in two recent studies on Pseudomonas bacteremia [10, 12], and this factor might also confound the results of former studies. Pertinently, Kang et al. [10] observed a trend towards higher mortality rates as the interval before appropriate treatment administration increased; thus, our trial population offered a unique opportunity to adequately control for this major confounding factor when evaluating the attributable mortality of resistant infections.
To date, no data on increased virulence of resistant Pseudomonas strains have been published. Virulence factors of this bacterium include: a type-III secretion system that confers the ability to inject toxins into host cells; quorum-sensing systems; a complex regulatory circuit involving cell-to-cell signaling which enables P. aeruginosa to regulate genes in a density-dependent manner through the production of autoinducers and secretion of various toxins, such as elastase, leukocidins, exotoxin A, and the diffusible pyocyanin pigment [25]. Additionally, these virulence factors sometimes trigger an exaggerated immune response, which participates in the bacterium-induced injury targeted at the lungs and other organs [25].
Host-related factors that might adversely affect outcome of infections due to resistant bacteria include more comorbidities, longer hospital stays, or patients' immunocompromised status at the time of infection onset [11, 14, 26, 27, 28, 29, 30]. In this study, we found no significant differences between ICU admission characteristics of the patients who would develop Pseudomonas VAP, except a non-significant trend towards a higher rate of underlying rapidly or ultimately fatal conditions in the PRPA group; however, the more severely ill status (higher SAPS II, SOFA, and radiological scores) at VAP onset and the higher crude mortality rate of our PRPA group are intriguing. Whether these higher morbidity scores and crude mortality rates for PRPA strains reflect more aggressive bacterial virulence factors, or that these bacterial strains found their niche in more acutely ill patients, remains to be determined.
Apart from ICU or in-hospital mortality, other significant outcomes also need to be assessed when evaluating the impact of antimicrobial resistance. The economic burden of such infections is heavy, due to prolonged hospitalization leading to higher care costs [6, 31]. Carmeli et al. [5] reported that emergence of resistance in Pseudomonas strains during the hospital stay was associated with a longer stay and an average increased cost of almost US $12,000. In the present study, we did not observe longer hospital stays or durations of MV, either for the whole cohort or when analyses were restricted to survivors being discharged. Similarly, rates of VAP recurrence, either superinfection or relapse, were comparable for our PRPA- and PSPA-infected patients.
Several limitations of the present study should be acknowledged. Firstly, we did not record Pseudomonas susceptibility to other antimicrobial agents, such as quinolones, aminoglycosides, carbapenems or third-generation antipseudomonal cephalosporins. Notably, resistance to at least one of these drugs was observed in 3–22% of PSPA strains in an earlier study [14]. The impact of antibiotic resistance on Pseudomonas VAP outcomes might be different for those antibiotics. Indeed, Kang et al. [11] recently observed that bloodstream infections due to imipenem-resistant Pseudomonas strains had the highest mortality rate, when compared with bacteremia due to piperacillin-, ceftazidime-, or ciprofloxacin-resistant strains. Secondly, since most patients with early onset VAP, immunocompromised status or a high probability of death (defined as a SAPS II > 65) were excluded from the PNEUMA trial, our conclusions may not be applicable to all patients developing Pseudomonas VAP. Thirdly, antibiotic-treatment duration was not the same for every patient (some patients were treated for 8 or 15 days in the PNEUMA trial); however, pertinently, treatment duration was not associated with 28-day mortality for patients with PSPA or PRPA VAP in this study. Finally, we cannot exclude that piperacillin-resistance might have been retained in the multivariable model predicting 28-day mortality if more patients had been included and thus the power of the study had been increased; nonetheless, our study is by far the largest to date to evaluate the impact of piperacillin resistance on PseudomonasVAP.
Conclusion
In conclusion, we observed that for patients with Pseudomonas VAP benefiting from appropriate empiric antibiotics, piperacillin-resistance was associated with more severe disease at VAP onset and higher 28-day crude mortality; however, after controlling for confounders, piperacillin resistance was no longer significantly associated with 28-day mortality. The VAP recurrence rates and durations of ICU stay and MV did not differ for susceptible and resistant strains. Whether this more severely ill status at VAP onset is due to bacterium- or host-related factors remains to be determined. Finally, early identification of patients with risk factors favoring antibiotic-resistant infections, such as more severe comorbidities, multiple hospitalizations, or prior antibiotic use and good knowledge of the bacterial ecology of the department in which the bacterium is isolated, are of utmost importance when initiating an empiric antibiotic regimen covering these highly resistant bacterial strains. This empiric antibiotic regimen may be de-escalated when results of microbiological sample cultures become available 48–72 h later.
References
Chastre J, Fagon JY (2002) Ventilator-associated pneumonia. Am J Respir Crit Care Med 165:867–903
Crouch-Brewer S, Wunderink RG, Jones CB, Leeper KV Jr. (1996) Ventilator-associated pneumonia due to Pseudomonas aeruginosa. Chest 109:1019–1029
Fagon JY, Chastre J, Domart Y, Trouillet JL, Gibert C (1996) Mortality due to ventilator-associated pneumonia or colonization with Pseudomonas or Acinetobacter species: assessment by quantitative culture of samples obtained by a protected specimen brush. Clin Infect Dis 23:538–542
National Nosocomial Infections Surveillance (NNIS) (2004) Report, data summary from January 1992 through June 2004, issued October 2004. Am J Infect Control 32:470–485
Carmeli Y, Troillet N, Karchmer AW, Samore MH (1999) Health and economic outcomes of antibiotic resistance in Pseudomonas aeruginosa. Arch Intern Med 159:1127–1132
Cosgrove SE, Carmeli Y (2003) The impact of antimicrobial resistance on health and economic outcomes. Clin Infect Dis 36:1433–1437
Blot S, Vandewoude K, De Bacquer D, Colardyn F (2002) Nosocomial bacteremia caused by antibiotic-resistant gram-negative bacteria in critically ill patients: clinical outcome and length of hospitalization. Clin Infect Dis 34:1600–1606
Blot S, Vandewoude K, Hoste E, Colardyn F (2003) Reappraisal of attributable mortality in critically ill patients with nosocomial bacteraemia involving Pseudomonas aeruginosa. J Hosp Infect 53:18–24
Aloush V, Navon-Venezia S, Seigman-Igra Y, Cabili S, Carmeli Y (2006) Multidrug-resistant Pseudomonas aeruginosa: risk factors and clinical impact. Antimicrob Agents Chemother 50:43–48
Kang CI, Kim SH, Kim HB, Park SW, Choe YJ, Oh MD, Kim EC, Choe KW (2003) Pseudomonas aeruginosa bacteremia: risk factors for mortality and influence of delayed receipt of effective antimicrobial therapy on clinical outcome. Clin Infect Dis 37:745–751
Kang CI, Kim SH, Park WB, Lee KD, Kim HB, Kim EC, Oh MD, Choe KW (2005) Risk factors for antimicrobial resistance and influence of resistance on mortality in patients with bloodstream infection caused by Pseudomonas aeruginosa. Microb Drug Resist 11:68–74
Micek ST, Lloyd AE, Ritchie DJ, Reichley RM, Fraser VJ, Kollef MH (2005) Pseudomonas aeruginosa bloodstream infection: importance of appropriate initial antimicrobial treatment. Antimicrob Agents Chemother 49:1306–1311
Raymond DP, Pelletier SJ, Crabtree TD, Evans HL, Pruett TL, Sawyer RG (2003) Impact of antibiotic-resistant Gram-negative bacilli infections on outcome in hospitalized patients. Crit Care Med 31:1035–1041
Trouillet JL, Vuagnat A, Combes A, Kassis N, Chastre J, Gibert C (2002) Pseudomonas aeruginosa ventilator-associated pneumonia: comparison of episodes due to piperacillin-resistant versus piperacillin-susceptible organisms. Clin Infect Dis 34:1047–1054
Chastre J, Wolff M, Fagon JY, Chevret S, Thomas F, Wermert D, Clementi E, Gonzalez J, Jusserand D, Asfar P, Perrin D, Fieux F, Aubas S (2003) Comparison of 8 vs 15 days of antibiotic therapy for ventilator-associated pneumonia in adults: a randomized trial. J Am Med Assoc 290:2588–2598
McCabe WR, Jackson GG (1962) Gram-negative bacteremia. Arch Intern Med 110:847–864
Le Gall JR, Lemeshow S, Saulnier F (1993) A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. J Am Med Assoc 270:2957–2963
Vincent JL, Moreno R, Takala J, Willatts S, Mendonca A de, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22:707–710
Fagon JY, Chastre J, Novara A, Medioni P, Gibert C (1993) Characterization of intensive care unit patients using a model based on the presence or absence of organ dysfunctions and/or infection: the ODIN model. Intensive Care Med 19:137–144
Weinberg PF, Matthay MA, Webster RO, Roskos KV, Goldstein IM, Murray JF (1984) Biologically active products of complement and acute lung injury in patients with the sepsis syndrome. Am Rev Respir Dis 130:791–796
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R (1994) The American-European Consensus Conference on ARDS. definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 149:818–824
Comite de l'Antibiogramme de la Societe Francaise de Microbiologie report (2003) Int J Antimicrob Agents 21:364–391
Katz MA (1999) Mutivariate analysis. Cambridge University Press, New York
Spanik S, Krupova I, Trupl J, Kunova A, Novotny J, Mateicka F, Pichnova E, Sulcova M, Sabo A, Jurga L, Krcmery Jr VV (1999) Bacteremia due to multiresistant Gram-negative bacilli in neutropenic cancer patients: a case-controlled study. J Infect Chemother 5:180–184
Sadikot RT, Blackwell TS, Christman JW, Prince AS (2005) Pathogen-host interactions in Pseudomonas aeruginosa pneumonia. Am J Respir Crit Care Med 171:1209–1223
Cao B, Wang H, Sun H, Zhu Y, Chen M (2004) Risk factors and clinical outcomes of nosocomial multi-drug resistant Pseudomonas aeruginosa infections. J Hosp Infect 57:112–118
Arruda EA, Marinho IS, Boulos M, Sinto SI, Caiaffa HH, Mendes CM, Oplustil CP, Sader H, Levy CE, Levin AS (1999) Nosocomial infections caused by multiresistant Pseudomonas aeruginosa. Infect Control Hosp Epidemiol 20:620–623
Defez C, Fabbro-Peray P, Bouziges N, Gouby A, Mahamat A, Daures JP, Sotto A (2004) Risk factors for multidrug-resistant Pseudomonas aeruginosa nosocomial infection. J Hosp Infect 57:209–216
Harris AD, Perencevich E, Roghmann MC, Morris G, Kaye KS, Johnson JA (2002) Risk factors for piperacillin-tazobactam-resistant Pseudomonas aeruginosa among hospitalized patients. Antimicrob Agents Chemother 46:854–858
Hsu DI, Okamoto MP, Murthy R, Wong-Beringer A (2005) Fluoroquinolone-resistant Pseudomonas aeruginosa: risk factors for acquisition and impact on outcomes. J Antimicrob Chemother 55:535–541
Shorr AF, Combes A, Kollef MH, Chastre J (2006) Methicillin-resistant Staphylococcus aureus prolongs intensive care unit stay in ventilator-associated pneumonia, despite initially appropriate antibiotic therapy. Crit Care Med 34:700–706
Acknowledgements
The PNEUMA trial was supported by a research grant from the Délégation à la Recherche Clinique, Assistance Publique-Hopitaux de Paris (PHRC AOM 97147). The PNEUMA Trial Group included the following investigators (French centers): A. Alvarez, C. Brun-Buisson, F. Stéphan (Hôpital Henri-Mondor, AP-HP), P. Alquier, P. Asfar (CHRU Angers), F. D'Athis (Hôpital Lapeyronnie, Montpellier), P.F. Perrigault, P. Colson, S. Aubas (Hôpital A.-de-Villeune, Montpellier), P. Corne, O. Jonquet (Hôpital Gui-de-Chauliac, Montpellier), J.P. Bedos (CHG de Versailles, Le Chesnay), F. Blot, G. Nitenberg (Institut Gustave-Roussy, Villejuif), J. Bocquet, P.E. Bollaert (Hôpital Général Nancy), F. Brivet, C. Legall, G. Simonneau (Hôpital de Clamart, AP-HP), R. Bronchard, J. Marty, H. Mal, M. Fournier (Hôpital Beaujon, AP-HP), M. Canonne (Hôpital Les Feugrais, Elbeuf), Y. Castaing (Hôpital Pellegrin Tripode, Bordeaux), J. Régnier, E. Clementi (Hôpital les Audaries, La-Roche-sur-Yon), J.M. Coulaud (CHI Montfermeil), Y. Domart (Centre Hospitalier, Compiègne), P. Gajdos, J Gonzalez (Hôpital Raymond Poincaré, AP–HP), B. Garo, J.M. Boles (Hôpital de la Cavale Blanche, Brest), R. Gauzit (Hôpital Jean-Verdier, AP-HP), C. Gervais, E. de la Coussaye (Hôpital Georges-Doumergue, Nîmes), S. Guyomarch, F. Zéni, (Hôpital Bellevue, Saint-Etienne), A. Jaeger (Hôpital Hautepierre, Strasbourg), P. Kalfon, F. Thomas (Hôpital des Diaconesses, Paris), J. Hayon, J.L. Ricome (CHG, St-Germain-en-Laye), G. Girault, G. Bonmarchand, D. Huchon, B. Veber, D Jusserand (Hôpital Charles-Nicolle, Rouen), J.C. Lacherade, H. Outin (CHI, Poissy), C. Lamer (Institut Montsouris, Paris), M.J. Laisné (Hôpital Lariboisière, AP-HP), A. Rabbat (Hôpital Hotel-Dieu, AP-HP), B. Schlemmer (Saint-Louis, AP-HP), E. Maury, G. Offenstadt (Hôpital Saint-Antoine, AP-HP), K. Nourdine, J.C. Ducreux (CHG, Roanne), J.L. Pallot (CHI, Montreuil), A. Tenaillon, D. Perrin (Hôpital Louise-Michel, Évry), E. Pigné, D. Dreyfuss (Hôpital Louis-Mourier, AP-HP), M. Pinsart (CH, Dieppe), C. Richard, D. Wermert (Hôpital du Kremlin-Bicêtre, AP-HP), A. Roch, J.P. Auffray (Hôpital Sainte-Marguerite, Marseille), M. Slama (Centre Hospitalier Sud, Amiens), J.P. Sollet, G. Bleichner (Hôpital V.-Dupouy, Argenteuil), F. Thaler, P. Loirat (Hôpital Foch, Suresnes), G. Trouillet (Centre Hospitalier, Pontoise), D. Villers (Hôtel-Dieu, Nantes), M. Wolff, B. Régnier, C. Paugam, J.M. Desmonts (Hôpital Bichat-Claude-Bernard, AP-HP), J.L. Diehl, A. Novara, J.Y. Fagon (HEGP, AP-HP), J.L. Trouillet, C. Gibert, and J. Chastre (Hôpital de la Pitié-Salpêtrière, AP-HP).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Combes, A., Luyt, CE., Fagon, JY. et al. Impact of piperacillin resistance on the outcome of Pseudomonas ventilator-associated pneumonia. Intensive Care Med 32, 1970–1978 (2006). https://doi.org/10.1007/s00134-006-0355-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-006-0355-7